Association of pyogenic spondylitis with congestive heart failure in Korea: a nationwide longitudinal cohort study
Article information
Abstract
Objective
The purpose of this nationwide longitudinal follow-up study was to investigate the risk of congestive heart failure (CHF) in pyogenic spondylitis (PS) patients in Korea.
Methods
A total of 628 patients were enrolled in the PS group from January 1, 2004 to December 31, 2015 from the National Health Insurance Service Health Screening cohort. PS was identified using the International Classification of Disease, 10th revision codes M46.2–M46.8 and M49.2–M49.3. The control group consisted of 3,140 subjects with 1:5 age- and sex-stratified matching. The 12-year CHF incidence rates in the PS and control groups were compared by the Kaplan-Meier method. The hazard ratio of CHF was estimated by Cox proportional-hazards regression analysis.
Results
During the 12-year follow-up period, 16 patients (2.55%) in the PS group and 43 (1.47%) in the control group developed CHF. The hazard ratio of CHF in the PS group was 6.32 (95% confidence interval [CI], 3.39–11.81) after adjusting for sex and age. The hazard ratio of CHF in the PS group was 6.49 (95% CI, 3.47–12.15) after adjusting for sex, age, and income. The hazard ratio of CHF in the PS group was 6.58 (95% CI, 3.50–12.40) after adjusting for sex, age, income, and comorbid medical disorders. In subgroup analyses, all subgroups showed higher CHF incidence rates in the PS group than in the control group.
Conclusion
Our nationwide longitudinal study shows a higher incidence rate of CHF in PS patients.
Introduction
Pyogenic spondylitis (PS) is an infection of the spine associated with severe morbidity and mortality [1]. It is an uncommon but life threatening disease which encompasses a broad range of clinical entities, including pyogenic spondylodiscitis, septic discitis, vertebral osteomyelitis, and epidural abscess [2]. PS patients have a higher risk of death due to cardiovascular diseases such as ischemic heart diseases and stroke [3]. Thus far, there has been no nationwide or large data-based study of the relationship between congestive heart failure (CHF) and PS. Our nationwide longitudinal follow-up study is not only the largest data thus far but also includes possible confounding factors, such as hypertension, diabetes, and dyslipidemia. The aim of the present study is to assess the risk of CHF in PS patients in Korea.
Material and Method
Data source
The National Health Insurance Service (NHIS) database, which covers 97% of the population in South Korea, was used for this study. All healthcare providers must submit medical claims to the NHIS for review and reimbursement. The NHIS provides annual or biannual health examinations for non-office or office workers aged >40 years, respectively. The collected patient data (e.g., demographic profiles, health insurance claims data, death certificates, disability certificates, and national health check-up results) are stored in the National Health Information Database (NHID). Representative data from the NHIS’s longitudinal cohort are publicly available for research purposes. The Sample Research Cohort Database [4,5] and the NHIS-HEALS [6] cohort database contain patient data collected dating back to 2002, statistically sampled from the NHID. The data in this study were obtained from the NHIS-HEALS cohort from 2004 to 2015.
The present study was approved by the institutional review board (IRB) of the CHA University, CHA Bundang Medical Center (IRB No. 2020-01-011). The need for informed consent was waived because the data consist of de-identified secondary data released for research purposes.
Study design
The PS group consisted of subjects who were newly diagnosed with PS (International Classification of Disease, 10th revision [ICD-10] Code M46.2–M46.8 and M49.2–M49.3) after January 1, 2004 and who also had a history of hospitalization. The CHF patients were defined by ICD-10 codes (I50) and hospitalization ≥1 [7–9]. Subjects in this study were followed from the first occurrence of CHF until death or end of follow-up (whichever occurred first). We evaluated the risk of CHF after adjusting for age, sex, and comorbidities (including hypertension, diabetes mellitus, and dyslipidemia). Information about preexisting comorbidities was obtained by retrieving all ambulatory medical care and inpatient records from the NHIS-HEALS cohort database.
Establishment of study cohort
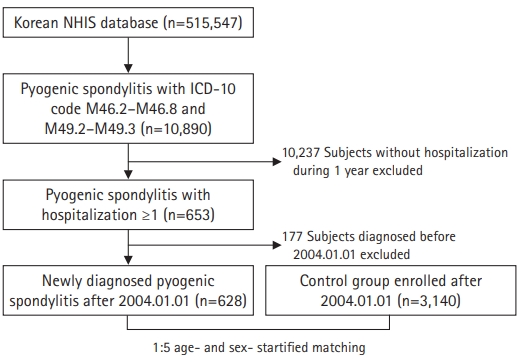
We extracted 10,890 PS subjects from a total of 515,547 patients in the NHIS-HEALS cohort. After removing 10,237 subjects without a history of hospitalization, 653 patients in total remained. Another 177 subjects who were diagnosed with PS before January 1, 2004 were excluded. Ultimately, 628 subjects were included in our base cohort. Through a 1:5 age- and sex-stratified matching performed by a greedy digit match algorithm [10], 3,140 subjects were included in the control group. Subjects in both groups were followed up to December 31, 2015 (Fig. 1).
Statistical analysis
The Kaplan-Meier method was used to estimate the CHF-free survival probabilities in the PS and control groups. The mean differences in the demographic characteristics and comorbidities between the two groups were compared using the chi-square test and Student t-test. The Wilcoxon’s log rank test was used to evaluate the differences in disease-free survival of the two groups. Multivariate analyses in the Cox proportional hazard regression model were conducted to estimate the effect of PS on CHF. Three Cox proportional hazard regression models were used in this study. Model 1 estimated the CHF incidence after adjusting for sex and age. In Model 2, age, sex, and income (low income was defined as the composite of the lowest quartile of yearly income in addition to medicare beneficiaries [11,12]) were adjusted. In Model 3, age, sex, income, and other comorbidities were adjusted. The analyses were performed using R software (ver. 3.3.3).
Results
Characteristics of the PS and control groups
The PS group consisted of 628 patients during the study period. Males constituted 51.4% of this group, and females 48.6%. The mean age of the patients was 59.09±9.35 years old. There were significant differences between the two groups in the prevalence of diabetes mellitus (P<0.01) (Table 1).
CHF in the PS and control groups
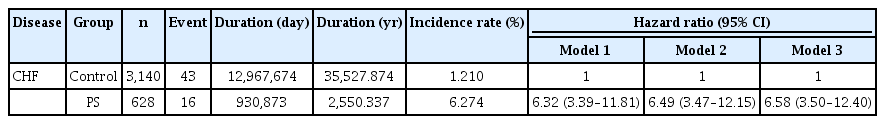
The CHF incidence rate in the PS group was significantly higher than that in the control group (P=0.05, Fig. 2). The Kaplan-Meier curves with cumulative hazards of CHF showed that the PS group was more likely to develop CHF than the control group. In a multivariate analysis of Cox proportional-hazards regression model 1, the hazard ratio of CHF in the PS group was 6.32 compared to the control group (95% confidence interval [CI], 3.39–11.81; Table 2). In a multivariate analysis of model 2, the hazard ratio of CHF in the PS group was 6.49 (95% CI, 3.47–12.15; Table 2). In a multivariate analysis of model 3, the hazard ratio of CHF in the PS group was 6.58 (95% CI, 3.50–12.40; Table 2).
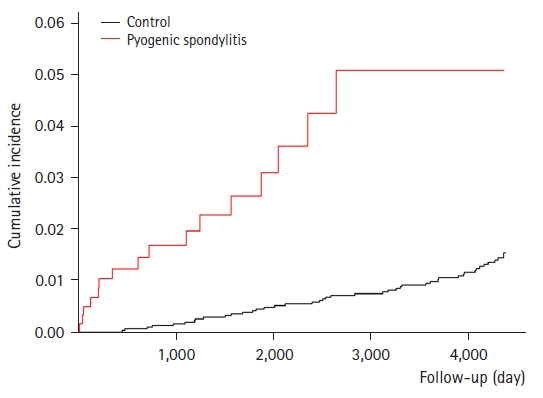
Kaplan-Meier curves with cumulative hazards of congestive heart failure in the pyogenic spondylitis and control groups.
Subgroup analysis of CHF in the PS and control groups
In both the male and female subgroups, CHF incidence rates were significantly different between PS and control group (95% CI, 2.05–16.81 and 2.78–14.71, respectively; Table 3). In both age subgroups (<65 and ≥65 years), CHF incidence rates were significantly different between the PS and control group (95% CI, 7.14–115.60 and 1.99–8.79, respectively; Table 3). In both the non-diabetes and the diabetes subgroups, CHF incidence rates were significantly different between the PS and control group (95% CI, 3.10–12.33 and 1.77–31.13, respectively; Table 3). In both the non-hypertension and the hypertension subgroups, CHF incidence rates were significantly different between the PS and control group (95% CI, 2.13–12.88 and 3.32–19.78, respectively; Table 3). In both non-dyslipidemia and the dyslipidemia subgroups, CHF incidence rates were significantly different between the PS and control group (95% CI, 3.27–13.32 and 1.55–25.93, respectively; Table 3).
Discussion
In this study, we compared the incidence of CHF in PS patients using claims data from the NHIS-HEALS cohort database and showed that PS was associated with an increased risk of CHF after adjusting for sex, age, income, and other comorbidities. Our study also showed that PS was associated with an increased prevalence of diabetes mellitus.
The reported incidences of PS are increasing due to increased life expectancy; the popularity of spinal, percutaneous invasive interventions; and advanced diagnostic methods [1,13–16]. In cases of hematogenous spreading pathogens in PS, Staphylococcus aureus is the predominant pathogen, accounting for half of non-tuberculous cases [17–19]. S. aureus, which is most often associated with healthcare contact and invasive procedures, is also the most common pathogen source of infective endocarditis (IE) [20]. An association between PS and IE has been frequently reported in early and recent reviews on spontaneous PS and raised the question of possibility of their relationship [21,22]. Based on our study, we may ask that the preexisting condition of IE may infect the spine while the IE deteriorates into CHF. We do not know whether PS occurs as a complication of IE or vice versa, but we do know based upon past studies that IE is an uncommon infection of the cardiac valves, where CHF is the most important complication [23]. Varma et al. [24] reported that 31 (78%) of 40 consecutive patients (aged 13–79, mean 44 years) with IE had CHF at presentation. Mills et al. [25] also reported that out of 144 patients with IE, 79 (55%) developed CHF. Thus, we suggest that the high incidence of CHF in PS may be related to the high association between IE and PS. Although there are several studies showing that CHF is one of the most common underlying diseases that accompanies PS [26,27], there has been no further studies discussing their relationship which is why studies of PS and its link to both IE and CHF should be conducted.
The CHF incidence rate was significantly higher in PS patients in the male/female, age <65 years/age ≥65 years, non-hypertension/hypertension, non-diabetes/diabetes and non-dyslipidemia/dyslipidemia subgroups (Table 3). Therefore, we can conclude that among PS patients, careful and thorough medical care should be advised for both male/female patients, hypertension/non-hypertension patients, diabetes/non-diabetes patients, and dyslipidemia/non-dyslipidemia patients.
Several limitations of this study should also be noted. First, due to the intrinsic limitations of the NHIS-HEALS cohort database, there is a lack of information with regard to pathogen types associated with PS patients. Second, clinical severity information and radiological data were not provided. Thus, patients’ current medical conditions were not accurately reflected [28]. Third, the data for this study was extracted from the NHIS which is why risk factors such as smoking, alcohol abuse, family history, and obesity were not included due to its limited access and the possible debate on accuracy. Nonetheless, this is the first nationwide longitudinal cohort study to assess the association between CHF and PS among Korean patients.
Conclusion
In conclusion, this nationwide longitudinal follow-up study shows an increased risk of CHF in PS patients. Based on this study, we emphasize that the increased risk of CHF should be kept in mind by those involved in the management of PS patients.
Notes
No potential conflict of interest relevant to this article was reported.
Author contribution
Acknowledgements
This work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2020R1I1A1A01072258). This work was also supported by a grant of Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and future Planning (NRF-2020R1F1A1069875).