Prevalence of Parkinson disease in Korea: a comprehensive analysis and regional comparison
Article information
Abstract
Objective
This study aimed to assess the prevalence of Parkinson disease (PD), a degenerative neurological condition, in Korea between 2016 and 2022.
Methods
For this comprehensive analysis, we utilized the Health Insurance Review and Assessment Service database, encompassing the entire population of Korea. A retrospective cross-sectional study design was employed to calculate the prevalence. We identified patients with diagnosis claim for PD (G20).
Results
The prevalence of PD increased from 96,499 in 2016 (186.3 per 100,000 persons) to 120,547 (232.6 per 100,000 persons) in 2022. The male-to-female ratio in 2022 was 42.6 to 57.4. Patients over 65 years old comprised a considerable portion of patients with PD. Larger institutions, especially hospitals, treated more patients than smaller institutions. Regional analysis showed substantial patient populations in areas such as Seoul (37,361), Busan (10,581), Gyeonggi-do (25,088), and Gyeongsangnam-do (7,211), among others. Young-onset PD accounted for 0.7% of total PD. The proportion of young-onset cases increased slightly over the years.
Conclusion
Our study provides evidence for a gradual increase in the prevalence of PD from 2016 to 2022 in Korea. The findings regarding PD in this article contribute to a better understanding of the disease’s epidemiology in the region and underscore the importance of ongoing monitoring and management strategies.
Introduction
Parkinson disease (PD) is a common progressive neurodegenerative condition, classified as a degenerative disorder, which becomes more prevalent with age. It affected approximately 0.4% of the population aged ≥50 years in 2019 [1], with reported incidence ranging from 80 to 678 individuals per 100,000 person-years [2–7]. According to a systemic review, Asia is known for a lower prevalence of PD across all age groups compared to other continents [8]. In Korea, the health insurance system has been under governmental control and has provided comprehensive coverage to the entire population since 1989 [2]. Referring to this paper, over 95% of the Korean population is covered by the national health insurance system, with the remaining receiving coverage through a Medical Aid program designed to assist those who are less fortunate. Therefore, the statistics provided by this institution offer information regarding the overall population of South Korea.
In this study, we conducted a thorough analysis of patient counts, regional prevalence data, as well as age and gender distributions of PD for the years 2016 and 2022 in Korea. Our primary objective is to comprehensively assess the prevalence of Parkinsonian disorders in Korea, specifically during the period spanning from 2016 to 2022. By shedding light on the dynamics of the diseases within the Korean population, this research aims to contribute to a deeper understanding of this neurodegenerative condition and its implications for public health in the country.
Material and Method
In this study, we utilized the Health Insurance Review and Assessment Service (HIRA) database, which encompasses the entire population of Korea. To assess the prevalence of PD (G20), we employed a retrospective cross-sectional study design. The data presented is based on statistics released by the HIRA and pertains to patients diagnosed with G20 code. Data collection and analysis encompass the period from 2016 to 2022 and include the following aspects: (1) annual patient counts: These figures represent the total number of patients diagnosed with G20 code for each year within the specified period (2016–2022); (2) patient counts by gender: The data differentiates patients based on gender, illustrating the distribution of G20 patients between males and females; (3) patient counts by age: The patients were categorized into age groups of 10-year intervals, and patients below 45-years-old were grouped as ‘Young-age’; (4) patient counts by the geographical location of healthcare facilities: This section examines the number of patients based on the location or geographical region of healthcare facilities. Specifically, it focuses on patients for whom G20 diagnostic codes were utilized; (5) patient counts by the type of medical institutions: This data examines patient counts categorized by the type or classification of medical institutions, providing insight into the distribution of patients among various institution types. The classifications include tertiary general hospital, general hospital, primary hospitals, private clinics, and others, such as clinics with specialized purposes like rehabilitation or comprehensive health checks. This data has been collected and analyzed to provide insights into the current status of Parkinsonian disorders in Korea.
Results
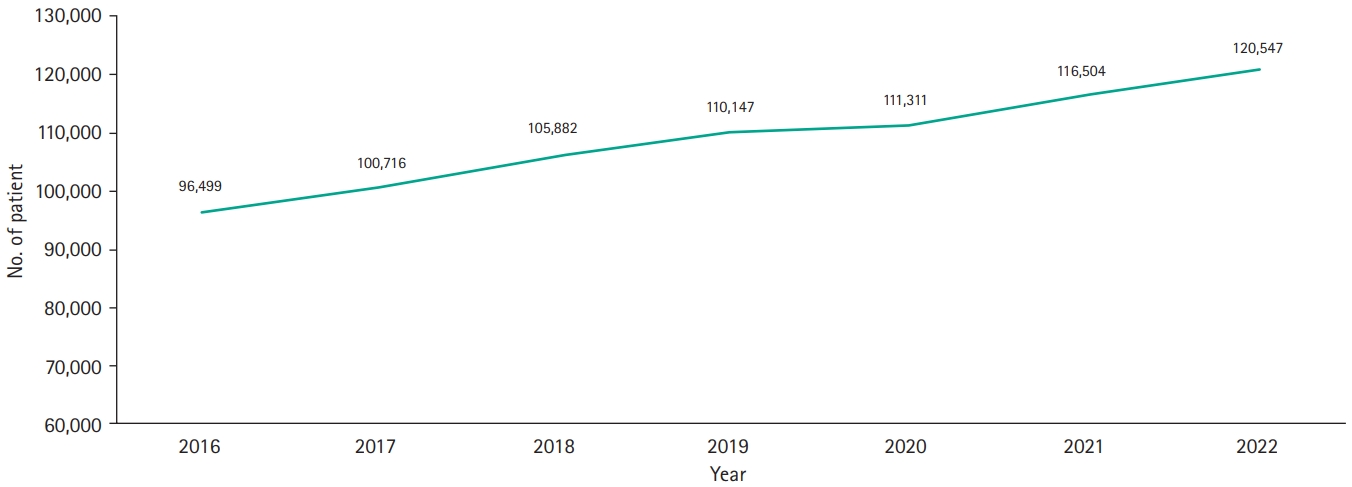
Prevalence of PD (G20) patients
The number of patients diagnosed with PD (G20) has gradually increased, from 96,499 individuals in 2016 to 120,547 in 2022 (Fig. 1). Over the years, the prevalence rate of PD has also risen, going from 186.6 per 100,000 persons in 2016 to 233.7 per 100,000 persons in 2022.
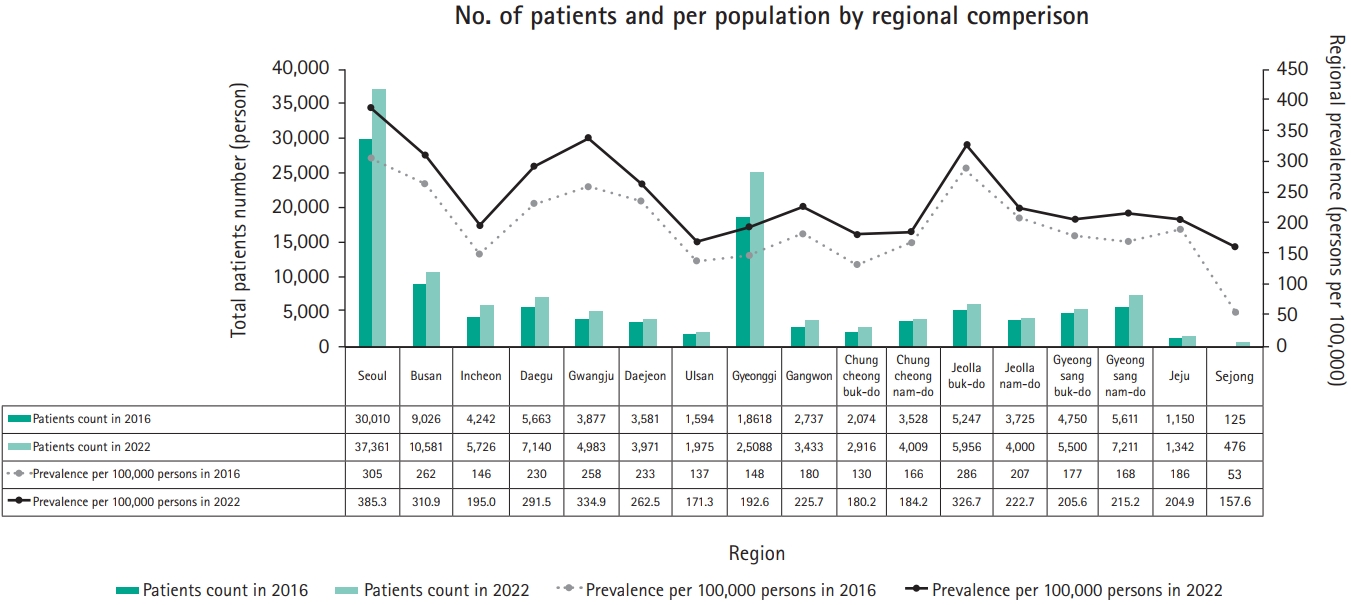
Regional distribution of PD (G20)
The number of PD patients increased in all provinces of Korea, accompanied by rising prevalence rates. Notably, the highest number of patients was concentrated in Seoul and Gyeonggi Province. When calculating prevalence relative to each region's population, Seoul exhibited the highest rate (385.3 per 100,000), followed by Gwangju (334.9 per 100,000) and Jeollabuk-do (326.7 per 100,000) (Fig. 2). In 2016, the trend was similar, although Jeollabuk-do’s prevalence slightly exceeded that of Gwangju, indicating consistent high prevalence in that specific region.
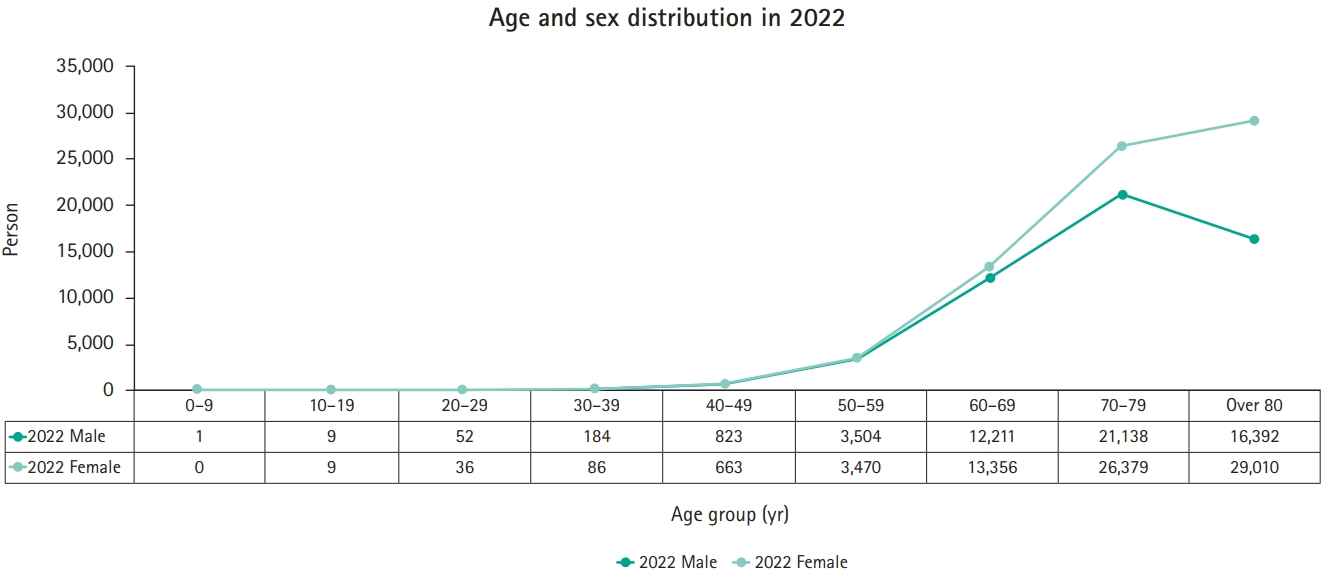
Male-to-female ratio of PD (G20)
In 2022, the male-to-female ratio among PD patients was 42.6:57.4. Among male patients, the highest number of PD cases was observed in the 70 to 79 age group, decreasing in the over 80 age group (Fig. 3). Among female patients, the trend mirrored that of male patients from 2016 to 2020. However, in 2021–2022, more patients were over 80 years old among females (Fig. 3). Until the age of 60, the number of PD patients was similar in males and females, but in older age groups, female patients outnumbered their male counterparts.
Distribution of treated medical institutions of PD (G20)
In 2022, patients were distributed among different types of treated medical institutions as follows: primary hospitals 27,356 (22.7%), general hospital 40,487 (33.6%), tertiary general hospital 55,181 (45.8%), private clinics 22,277 (18.5%), and others 97 (0.1%). If the numbers for each type of medical institutions are added, they exceed the total number of PD patients in 2022, indicating that some patients visited multiple types of institutions. Larger medical institutions had more patients. The number of days of visits was as follows: primary hospitals 3,357,261 (83.5%), general hospitals 269,983 (6.7%), tertiary general hospitals 261,913 (6.5%), private clinics 132,770 (3.3%), and others 487 (0.01%). Unlike the patient count, primary hospitals and general hospitals had a larger number than tertiary general hospitals. In regional aspect, significant patient concentrations were observed regionally in Seoul (37,361), Busan (10,581), Gyeonggi-do (25,088), Gyeongsangnam-do (7,211), among others.
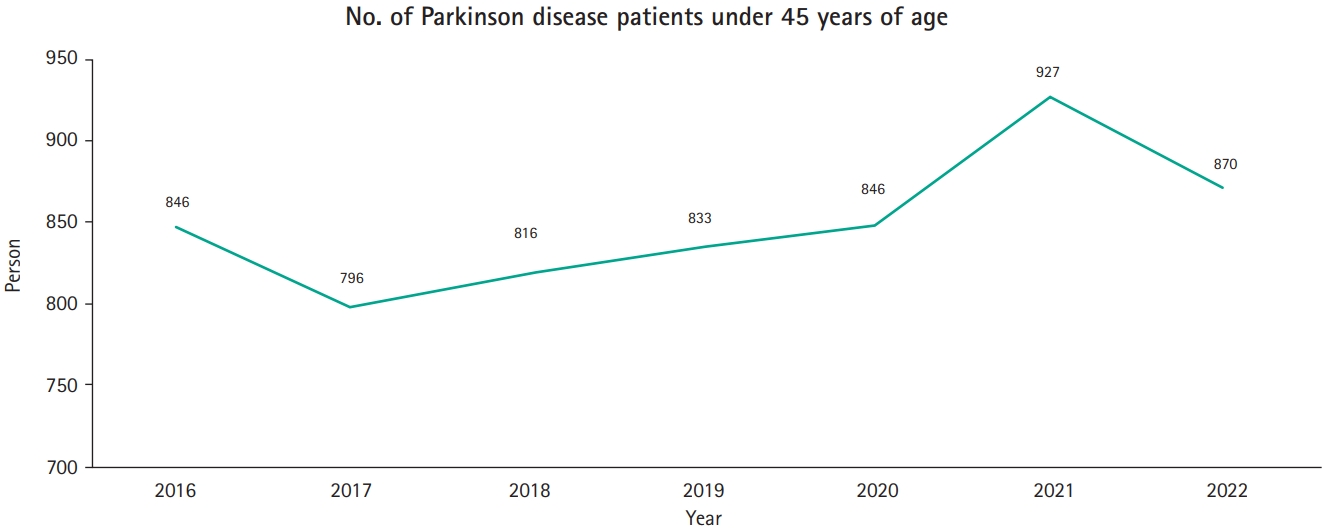
Young-age PD (G20)
Among the population with young-age onset PD (below 45 years), there were 870 cases, accounting for 0.7% of the total PD cases in 2022. The annual trend of the total number of young-age onset PD patients (below 45 years) is shown in (Fig. 4). The percentage of young-age onset patients as a proportion of the total number of patients was 0.88% in 2016, 0.79% in 2017, 0.77% in 2018, 0.76% in 2019, 0.76% in 2020, and 0.80% in 2021 for PD (G20).
Discussion
While the prevalence of PD varies from year to year, there has been a consistent upward trend, which may continue in the future [9]. According the statistics provided by HIRA, the incidence of PD cases in Korea witnessed a substantial rise, surging from 44,619 cases in 1995 to 96,229 cases in 2000. In the study conducted by Kim and Sohn [10], assuming that each patient adheres to their prescribed treatment regimen for the entire insurance coverage period, the average number of healthcare visits in the year 2000 amounted to 11. This calculation leads us to an estimated population of approximately 8,600 individuals affected by PD. According to the study of Kim and Sohn [10], the prevalence was 19 per 100,000 in 2000. The figure was significantly lower than the statistics reported in Japan during 2003–2004, in which prevalence was 180.3 per 100,000 people [11].
The prevalence of PD surged from 156.9 per 100,000 individuals in 2012 to 181.3 per 100,000 in 2015 [1]. The trend has exhibited some fluctuations, as observed by Han et al. in their study of PD and drug-induced parkinsonism (DIP) prevalence and incidence in Korea from 2012 to 2015 [2]. PD prevalence increased from 156.9 to 181.3 per 100,000 persons, while incidence decreased from 35.4 to 33.3 per 100,000 person-years. In contrast, DIP prevalence and incidence rose from 7.3 to 15.4 per 100,000 persons and 7.1 to 13.9 per 100,000 person-years, respectively. This indicates changing trends in PD and DIP.
However, according to our study, the prevalence of PD surged even further, from 186.3 per 100,000 persons in 2016 to 233.7 per 100,000 individuals by 2022, reaching a record high.
Regarding age, Pringsheim et al.’s meta-analysis [8] revealed higher PD prevalence in North America, Europe, and Australia compared to Asia, with rates increasing with age. Males aged 50 to 59 had a higher prevalence than females. Overall, PD prevalence rose with age. In our study, the age-specific prevalence continuously increased with age in male patients. However, in female patients, age-specific prevalence increased until the 75 to 79 age group but decreased in the over 80 years group. This result corresponds with another study conducted in Korea using the same HIRA data for the years 2012–2015 [2]. The is believed to be due to higher life expectancy among women and the occurrence of many other diseases in the elderly, which reduce the necessity for PD treatment. Our study relies on data from HIRA, which is recorded only when a diagnosis code is claimed. Therefore, if patients receive treatment under a different diagnosis, the number of patients is not recorded.
Additionally, the percentage of young-age onset patients in total of PD (below 45 years) is very low in this study. This implies that age is a stronger risk factor in PD.
Choi [12] reported on the 2012 population and the 2010 Population and Housing Census data provided by Statistics Korea, examining regional population distribution and concentration in the capital area. The findings highlighted several key observations: at the provincial level, Gyeonggi-do (Gyeonggi Province) had the highest population, while Seoul exhibited the highest population density. However, when considering the total dependency ratio, which includes both the population aged 65 and older and the population aged 14 and younger, Seoul demonstrated the lowest ratio. Relatively, cities like Daegu and Busan, Gwangju, falling under a provincial category, along with nearby cities in Gyeongsang-do and Jeolla-do regions, exhibited a high proportion of elderly populations. This trend indicated that over time, regional disparities in aging populations increased. Furthermore, the overall regional populations in provincial cities declined over time, as there was a tendency for populations to concentrate in urban centers such as Seoul and the Gyeonggi-do metropolitan areas. The concentration of the population and the aging phenomenon in rural areas have significantly influenced the regional prevalence rates of PD.
Research has shown that there is a connection between an aging population and the prevalence of PD, and it's worth exploring whether the concentration of elderly individuals in specific regions can lead to higher disease prevalence in those areas. Seo et al. [13] conducted a study on the prevalence of PD in the elderly population of a newly industrialized city in a rural region of Korea in 1998. This study examined approximately 1.3% (4,700) of 362,625 adults (age >18 years) listed in the city register in 1998. About a quarter of the subjects were over 60 years old. In this study, the prevalence in this population was 0.37% (373 per 100,000 persons), and it increased with age, reaching 1.47% for those aged older than 60 years. In fact, all the subjects who were afflicted were over 60 years old. The results of our prevalence study are similar to those of studies carried out in Western countries.
The prevalence of PD exhibited the highest rates in Seoul, Gwangju, and Jeollabuk-do, in that order. This can be attributed to the fact that the reported prevalence is based on the locations of medical institutions where diagnosis codes were claimed, and these cities are home to many large medical facilities. Furthermore, cities like Gwangju and Jeollabuk-do have larger aging populations. In contrast, the regional prevalence in Sejong is notably low due to a lack of medical facilities and an older population.
One limitation of this study lies in its reliance on data based on diagnosis codes from the HIRA. This approach may introduce inaccuracies in cases where diagnosis codes are misapplied or when patients' residential locations do not align with the medical facilities they visited. Nevertheless, the significance of this study lies in its comprehensive analysis, encompassing data from nearly all patients with Parkinsonian disorders in Korea.
Conclusion
PD demonstrates a gradually increasing prevalence, which is anticipated to persist in the future, largely associated with the aging population trend. Furthermore, within Korea, the prevalence of PD varies significantly across regions. Hence, additional research is essential, not only considering the aging phenomenon and the distribution of healthcare institutions by region but also delving into the specific risk factors prevalent in each region.
Notes
No potential conflict of interest relevant to this article was reported.