Functional outcomes of surgically treated chronic subdural hematoma and the factors associated with outcomes: a retrospective study
Article information
Abstract
Objective
The incidence of chronic subdural hematoma (CSDH) and its peak age of occurrence are increasing with the rapid progression of population aging. Surgical treatment for symptomatic CSDH has shown favorable clinical outcomes (>80%). Since some recent reports have described unfavorable outcomes of surgical treatment of CSDH in older patients, we evaluated the functional outcomes of CSDH in older patients.
Methods
We retrospectively analyzed the functional outcomes of CSDH patients aged >60 years who underwent burr-hole surgery between January 2017 and December 2021. Using the modified Rankin scale (mRS), we analyzed the functional outcomes of burr surgery and investigated the factors affecting the surgical outcomes.
Results
In total, 172 patients (115 men and 57 women) were analyzed for the functional outcomes of surgery. Functional outcomes improved in 120 patients (69.8%) and worsened in 52 patients (30.2%). Age (P=0.046), preoperative mRS (P=0.002), and the presence of underlying disease (P=0.025) were factors affecting the postoperative functional status.
Conclusion
The decision regarding surgical treatment of CSDH in older patients should be made carefully, considering their preoperative functional status and underlying disease.
Introduction
Liquefied hematoma within the subdural space enclosed by a distinct outer membrane was defined as chronic subdural hematoma (CSDH) [1,2]. The mean age of CSDH patients was 76.8 years, and the male-to-female ratio was 3:1 for all age groups [3]. The annual incidence of CSDH is approximately 10 cases per 100,000 individuals [4,5], and older patients are susceptible to CSDH due to minor trauma associated with brain atrophy [6,7].
Surgical treatment is the primary approach for managing symptomatic CSDH, with 3 key techniques: twist-drill craniotomy, burr-hole craniotomy, and larger-opening craniotomy [8]. Among these, the burr-hole craniotomy stands as the most prevalent approach [9,10]. Surgical treatment of symptomatic CSDH can improve symptoms quickly and has favorable outcomes in more than 80% of patients [2].
As the global population trends toward advanced age, the overall incidence of CSDH is raising [11] accompanied by a shift in the peak onset age. A Japanese study indicated that the recent peak age of onset was shown to be the 80s [12]. In many recent reports, the long-term surgical outcomes of older patients with CSDH are unfavorable, and they argue that CSDH in older patients is no longer a benign disease [13–15]. Considering these aspects of research, we executed the clinical study analyzing the functional outcomes of burr-hole surgery for older CSDH patients.
Material and Method
Patients and materials
Electronic medical records (EMR) of patients aged over 60 years who received burr-hole surgery for CSDH at the Inha University Hospital between January 2017 and December 2021 were retrospectively reviewed. Among the 191 patients who underwent burr-hole surgery for CSDH during this period, 19 patients were excluded from the analysis due to incomplete medical records to evaluate the functional status of the patients. Consequently, the final analysis comprised 172 patients.
Functional outcomes of the surgical treatment were assessed by comparing pre- and postoperative modified Rankin score (mRS), a widely used criterion for evaluating functional outcomes [16]. Preoperative mRS was determined based on initially recorded mRS at the hospital visit, and the postoperative mRS was based on the mRS evaluated 3 months after burr-hole surgery. To compare pre and postoperative outcomes, we categorized patients into 2 groups: an “improved group” included patients whose mRS decreased after surgery, and a “Worsened group” those whose mRS exhibits no change or increased after surgery. A history of major symptoms, underlying disease, and preoperative antithrombotic medication use was specifically evaluated during hospitalization. Underlying diseases included previously diagnosed diseases, such as hypertension, diabetes mellitus (DM), hyperlipidemia (HL), cardiovascular disease (CVD), and cancer. Postoperative medications included statins and tranexamic acid.
The patient’s radiologic characteristics were evaluated based on midline shifting and thickness of hematoma at axial cut of computed tomography (CT). The midline shifting was quantified by measuring the distance from the linear connection line between anterior and posterior falx to the septum pellucidum. Thickness of hematoma was measured as the thickest width in the fronto-parietal convexity (Fig. 1).
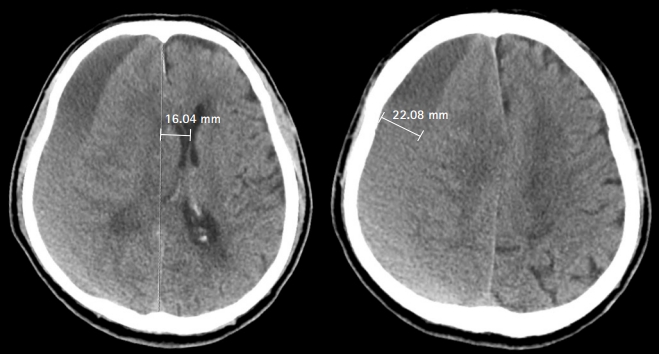
Measurement of midline shifting and thickness of hematoma on an axial computed tomography cut. The midline shifting was evaluated by calculating the distance between the line connecting the anterior and posterior falx with the septum pellucidum. The thickness of the hematoma was measured according to the greatest width of fronto-parietal convexity.
Surgical procedure
A single burr hole was made at the parietal eminence under general anesthesia. After dural incision, the outer membrane was opened, and a silicon tube was inserted 3 to 4 cm from outer membrane of dura into the hematoma cavity. And then silicon tube was connected to a closed drainage system. No evacuation or irrigation of the hematoma was performed. In the cases of septated CSDH, irrigation was performed after additional frontal burr hole was made. Drain removal was clinically determined based on the patient’s condition, amount of drainage, and improvement of midline shifting at CT scan.
Statistics
Clinical factors affecting functional outcomes were analyzed through logistic regression analysis. A univariate analysis was performed to examine the presence of an association between the clinically important variables and functional outcomes of the burr-hole surgery. A multivariate analysis was performed by including all variables utilized in univariate analysis since it judged to be clinically important factors for functional outcomes.
All statistical analyses and illustrations of the graphical figures were performed using the free software program R ver. 4.2.2 (The R Foundation), and a P-value of less than 0.05 was considered statistically significant.
Results
Characteristics of patients
The 172 patients who underwent burr-hole craniotomy for CSDH were included in this study. The patients had an average of 75.1±9.0 years (range, 60–120), with 115 males (66.9%) and 57 females (33.1%). The motor weakness was the predominant preoperative major symptom, affecting 90 patients (52.3%), followed by headache in 40 patients (23.3%).
A total of 147 patients (85.5%) had an underlying disease. Among them, the 70 patients had single disease (HNT or DM or HL, 56; CVD, 12; cancer, 2) and the 77 patients had 2 or more diseases. There were 55 patients of CVD and the 37 patients were taking antithrombotic agents due to CVD. The 14 patients prescribed the antithrombotic agents without the diagnosis of CVD. Mean follow-up duration was 11.6 months (range, 2–64) and the summary of the patient’s demographic and clinical characteristics is presented in Table 1.
Functional outcomes
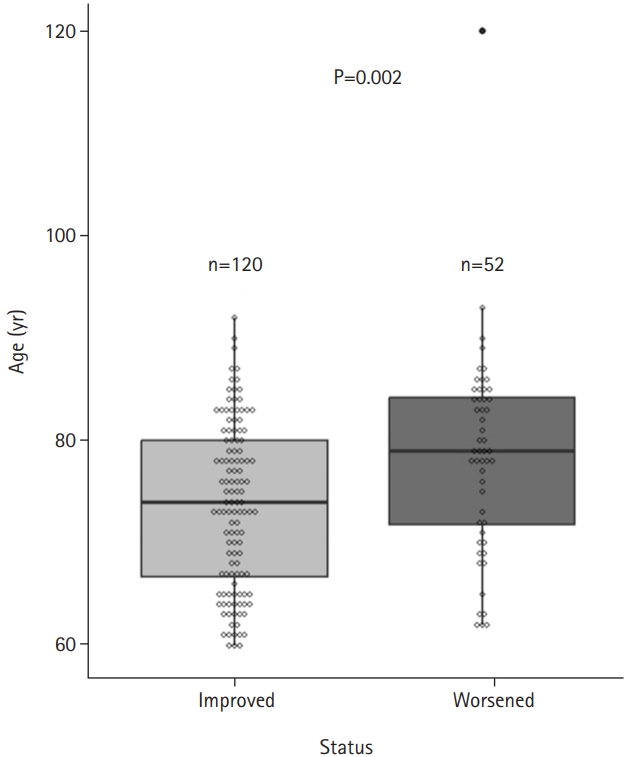
Following burr-hole surgery, 120 patients (69.8%) demonstrated improved status, whereas 52 patients (30.2%) exhibited worsened status (Fig. 2). The median age of improved group and worsened group was 74 and 79 years, respectively, and the age represented significant difference between 2 groups (P=0.002) (Fig. 3). Recurrence of CSDH requiring re-operations presented in 14 patients (8.1%), and there was no statistical difference in the age of recurred patients (P=0.059).
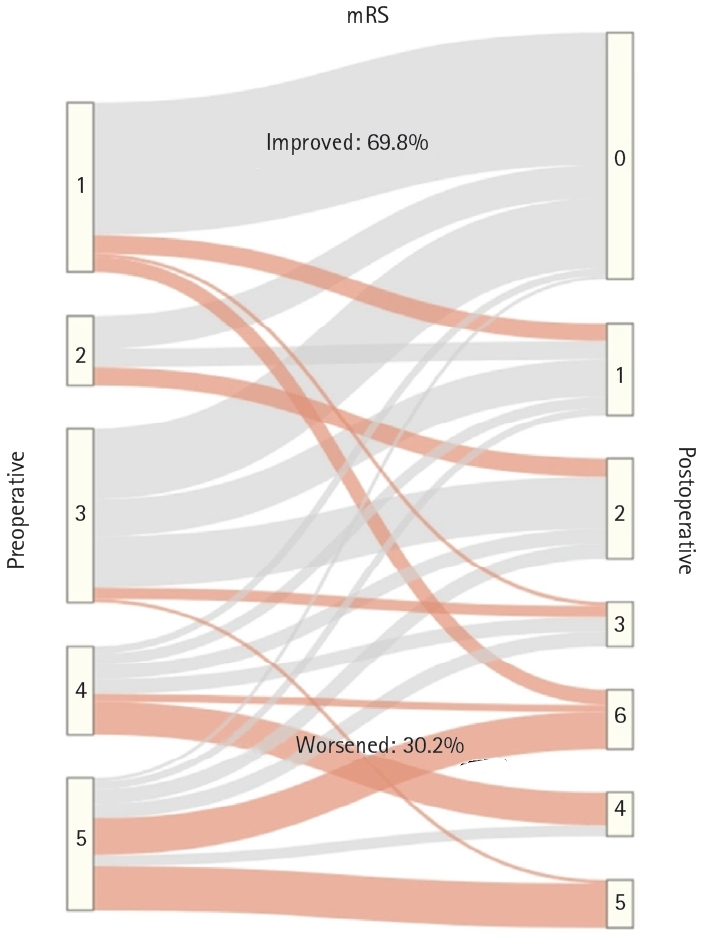
A Sankey diagram shows a comparison of preoperative functional status and postoperative functional status based on the modified Rankin scale (mRS) score. There were 120 patients (69.8%) whose status improved and 52 patients (30.2%) whose status worsened.
Radiological features
The average thickness of hematoma was 21.52 (range, 7.10–49.10) mm and the mean midline shifting was 8.2 (range, 0.7–18.6) mm. The postoperative pneumocephalus were observed in 152 patients (88.4%), while it was absent in 20 patients (11.6%).
Uni/multivariate analysis
Logistic regression analysis was conducted to evaluate the postoperative functional status. Age (odds ratio [OR], 1.05; 95% confidence interval [CI], 1.00–1.09; P=0.046), preoperative mRS (OR, 1.51; 95% CI, 1.16–1.97; P=0.002), and presence of underlying disease (OR, 4.64; 95% CI, 1.22–17.70; P=0.025) were identified as significant factors influencing outcomes in the functional status analysis. Preoperative antithrombotic and postoperative medications (statins and/or tranexamic acid) did not affect the postoperative functional status. Detailed results of the logistic regression analysis for functional outcomes are presented in Table 2.
Discussion
Burr-hole surgery for symptomatic CSDH quickly improved the patient’s symptoms and has favorable outcomes [2,8]. However, recent researches have raised doubts about the effectiveness of surgical treatment for older CSDH patients [13,15,17]. In this study, the improvement rate of functional status among CSDH patients aged over 60 years who underwent burr-hole surgery was recorded at 69.8%, which was lower than the improvement rate of 80% observed across all age group [2]. This result supports the argument that surgical treatment might be less advantageous for older patients with CSDH.
Former studies had indicated an increased recurrence rate of CSDH associated with preoperative antithrombic medication use [18–20]. However, in this study, preoperative antithrombotic medication did not significantly affect outcomes of functional status. Similarly, postoperative medications such as statins and tranexamic acid have been reported to effectively reduce postoperative recurrence in patients with CSDH [21–23]. However, the administration of postoperative medications (statins and/or tranexamic acid) did not affect functional outcomes. Since postoperative medication is not a standard treatment and there are controversial issues [24,25], our results will not be faulty.
Underlying disease have an impact on postoperative functional status. Among the patients, 85.5% of patients had underlying diseases, which is a general characteristic of older patients [26]. As the aging society progresses, the population of patients with underlying diseases is expected to gradually increase. Therefore, decision of surgical treatment for CSDH patients with underlying diseases needs to be cautious.
Regarding the assessment of mRS, potential errors might arise due to the fact that it was not evaluated by a single physician and relied on the EMR. However, the authors conducted a thorough review of the EMR, including main symptoms and postoperative status, leading to the assertion that the results are precise. In addition, as the postoperative mRS evaluation occurred 3 months after the burr-hole surgery, its ability to reflect the long-term functional status might be limited. Since the recovery time of functional status and long-term outcomes may vary between patients, set the appropriate follow-up period after surgery are important to evaluate the effectiveness of the procedure. In case of burr-hole surgery for CSDH, since the symptoms can improve rapidly, it seems the patient's condition remains similar at 1year compared to 3 months after burr-hole surgery.
We evaluated the radiologic characteristics of midline shifting and thickness of hematoma on preoperative CT. However, radiologic characteristics were not included in statistical analysis since the conscious level of patients were similar regardless of the amount of midline shifting and thickness of hematoma. Due to its retrospective nature, this study has inevitable limitations of selection bias and absence of control group. However, the results of the study are expected to help surgeon to decide reasonable decision making for burr-hole surgery. When more clinical data are accumulated, further research will be conducted.
Conclusion
The outcomes of surgical treatment may be less favorable among older patients with CSDH. Particularly, the decision for surgical treatment should be approached cautiously, considering both the preoperative functional status and underlying medical conditions.
Notes
No potential conflict of interest relevant to this article was reported.