Safety and effectiveness of the modified stent retrieval technique in elderly patients with secondary distal vessel occlusion
Article information
Abstract
Objective
This study aimed to investigate the efficacy and safety of the modified stent retrieval (STR) technique in solving the problem of newly migrated embolic particles during primary mechanical thrombectomy for acute large vessel occlusion (LVO), specifically in patients aged 65 and older. In order to minimize risk and enhance the success rate, a modified STR technique was developed, which enables control over the unsheathing level of the microcatheter. We investigated the safety and effectiveness of this technique in resolving distal vessel occlusion (DVO) resulting from migrated emboli in elderly patients.
Methods
Between January 2016 and February 2022, 16 patients (5.4% of 294 total patients) aged 65 and older, who presented with an acute LVO stroke in the anterior circulation and secondary migration of the embolus into M2, M3, A2, or A3 branches, underwent the modified STR technique.
Results
After recanalizing the primary LVO, secondary DVO occurred in 7/4/4/1 patients in M2/M3/A2/A3, respectively. The modified Thrombolysis in Cerebral Infarction (mTICI) score was 2a in 5 patients and 2b in 11 patients for LVO. The one-pass rate was 62.5% and the final recanalization rate of at least TICI 2c at the migrated DVO was 15 out of 16 patients (93.8%, mean duration, 25.2±13 minutes) without significant complications. A favorable functional outcome (modified Rankin Scale, 0–2) was achieved in 8 (50.0%) patients at 3 months.
Conclusion
The modified STR technique is simple and can improve the safety and effectiveness of recanalization in DVO caused by migrated emboli in elderly patients.
Introduction
Mechanical thrombectomy (MT) has proven to be a highly effective and beneficial treatment for acute large vessel occlusion (LVO) in elderly patients [1]. It has significantly higher recanalization rates compared to traditional medical management or intravenous (IV) thrombolysis alone. It allows for rapid and direct removal or fragmentation of the clot, restoring blood flow to the affected area of the brain. Several studies have demonstrated that endovascular therapy leads to improved clinical outcomes in geriatric patients with acute LVO [2,3]. It can reduce disability and dependence, increase the likelihood of functional independence, and improve overall quality of life compared to medical management alone.
However, it is reported rates ranging from 11% to 16% for secondary occlusion to occur during the procedure [4,5]. Unfortunately, the presence of new distal vessel occlusions (DVO) can significantly affect the final modified Thrombolysis in Cerebral Infarction (mTICI) score and functional disability in geriatric patients. For example, a distal middle cerebral artery occlusion causing aphasia or an anterior cerebral artery occlusion causing monoplegia can have a devastating impact on a patient's functional independence [6].
When it comes to perform the procedure in elderly patients, there are a few considerations such as the small caliber, fragility, and tortuous anatomy of the affected vessels which largely raise concerns about arterial traumas. To overcome these obstacles, the use of technical adjusting of the primary stent to reduce contact area can be considered to minimize the risk and achieve successful recanalization.
In this regard, we aimed to evaluate the safety and effectiveness of a modified stent retrieval (STR) technique for the removal of a new migrated emboli in the M2, M3, A2, and A3 segments during MT for acute LVO in elderly patients.
Material and Method
Patients
This retrospective study was approved by the Institutional Review Board of Kangdong Sacred Heart Hospital (IRB No. KANGDONG 2023-07-010), and all participants provided informed consent. A total of 16 patients (5.4% of the 294 patients) aged 65 and older, who experienced secondary embolic migration to the distal branch (M2, M3, or A2, A3) after the primary intervention for acute LVO stroke in the anterior circulation from January 2016 to February 2022 were enrolled. The emboli to new territory (ENT) were defined according to the standard angiographic anatomy. Eligibility criteria for the modified STR technique at the DVO were as follows: After achieving complete recanalization of the primary LVO with mTICI 2a or 2b score, the neurointerventionalist evaluated whether ENT affected the main blood supply to an eloquent area, if the device was accessible without vascular tortuosity or tension, and if retrograde filling into the ENT would not prevent further ischemic progression. Exclusion criteria included evidence of intracranial hemorrhage (IH) or low density on the initial computed tomography (CT) scan in the secondary migrated territory which was considered ineloquent area. For each patient, the following data was collected and reviewed: age, sex, risk factors, baseline modified Rankin Scale (mRS) score, National Institutes of Health Stroke Scale (NIHSS) score, Alberta Stroke Program Early CT Score (ASPECTS), use of tissue plasminogen activator (tPA), time from symptom onset to arrival at the hospital, time from symptom onset to femoral puncture, time from femoral puncture to successful recanalization, location of primary LVO, migrated DVO, total procedural time (divided into primary LVO and secondary DVO), primary thrombectomy devices, secondary stent retriever, modified STR technique attempts, final mTICI score with 2c, and other relevant information.
Modified STR technique
All mechanical thrombectomies were performed through femoral puncture while the patients were under conscious sedation. A balloon-guiding catheter (8 or 9-Fr BGC Cello/Medtronic, USA or 9-Fr Optimo/Medtronic, Irvine, CA, USA) or a non-balloon guiding catheter (Neuromax 6-F or Fubuki 7-F) was selected for the anterior circulation and placed as far distally as possible in the cervical internal carotid artery (ICA) of the occluded side, using a 5-F long angio-catheter for navigation. The primary LVO site was initially accessed using the Trevo XP ProVue 4×20 mm (Stryker Neurovascular, Fremont, CA, USA), Solitaire Platinum 4×20 mm (Medtronic, Dublin, Ireland), or Penumbra Reperfusion Catheter 5Max Ace 068. A microcatheter (Prowler Select Plus/Cordis, Dublin, OH, USA or Markman 27/Medtronic) was navigated to the point of occlusion, and super-selective angiography was performed to evaluate the length of thrombus and distal vascular nature. If ENT occurred in the DVO after successful recanalization of the primary LVO, either the Trevo XP ProVue 4×20 mm or Solitaire Platinum 4×20 mm retriever stent was applied. The deployed range was easily identified by the radiopaque wire or marker, respectively. The modified STR technique was used to remove the clot by adjusting the covered range of the stent, which involved partially re-sheathing the delivery catheter after fully unsheathing it. The microcatheter and microwire were maneuvered over the embolic lesion (Fig. 1A), and the radiopaque stent retriever was carefully deployed inside the thrombus by unsheathing the microcatheter (Fig. 1B). At this point, the waisted portion of the stent could be indicated by compression of the clot. After waiting for 2 minutes to allow the clot to engage with the stent, the microcatheter was gently pushed forward to partially re-sheath, reducing the physical friction between the parent artery and the stent (Fig. 1C) [7]. Resistance felt during the re-sheathing process indicated that the clot was in contact with the microcatheter. The partially re-sheathed stent was slowly retrieved into the guide catheter by pulling back, with careful monitoring of the motion of the parent artery and under balloon guiding inflation or proximal aspiration (Fig. 1D).
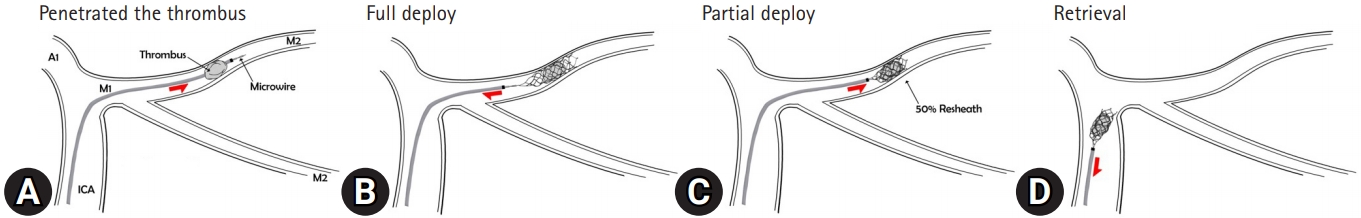
(A) A microcatheter and microwire move over an embolic lesion. (B) A radiopaque stent retriever is carefully deployed inside the thrombus by unsheathing the microcatheter. (C) After waiting for 2 min¬utes, the microcatheter is gently pushed forward to partially re-sheath. (D) The partially re-sheathed stent is slowly retrieved into the guide catheter by pulling back. ICA, internal carotid artery.
Complication and outcome
Procedure-related complications were recorded during the intra-angiography and post-procedural CT scans. Stenosis of the targeted vessel and a double contour layer after retrieval were defined as arterial vasospasm and dissection, respectively. Vessel perforation was determined if a contrast leak was noted due to incorrect navigation of the microcatheter and microwire. Post-procedural CT scans were used to identify intracerebral hemorrhages (ICH), classified as IH 1, 2 and parenchymal hemorrhage (PH) 1, 2 according to the European Cooperative Acute Stroke Study II classification system. Symptomatic ICH was defined as a worsening of clinical examination by ≥4 points on the NIHSS scale, in the presence of hemorrhage on the CT scan after treatment. The mTICI classification was used to define the primary LVO and secondary DVO before and after treatment. Successful revascularization was defined as an mTICI score of 2c or 3 and was determined by 2 blinded physicians based on the procedural process. Patients underwent magnetic resonance imaging (MRI) within 24 to 48 hours after the procedure to evaluate regional ischemic findings related to the ENT, which were classified as complete, partial, or none. Clinical outcomes were assessed using the NIHSS and mRS at discharge and 90 days after treatment. A good functional outcome was defined as an mRS score of ≤2 at 3 months.
Ethical approval
All procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Board of Kangdong Sacred Heart Hospital (IRB No. KANGDONG 2023-07-010) and Informed consent was obtained from all study participants.
Results
Within the study period, 16 out of 294 (5.4%) elderly patients with acute LVO in the anterior circulation who underwent MT developed ENT. All cases of DVO were managed using the modified STR technique. The demographic characteristics, device profiles, and procedural outcomes are summarized in Table 1. The mean age of the patients was 73.1 years, and 75.0% were women. The median baseline NIHSS score was 14.1±4.5, and 6 patients (37.5%) received IV tPA within the 4.5-hour time window. The median ASPECTS at baseline was 8.2±1.7, and collateral status on multiphase CT angiography showed good collateral flow in 4 cases, moderate flow in 5 cases, and poor flow in 7 cases. The primary occlusion site was observed in 7 patients at the ICA and in 9 patients at the M1 segment. Secondary DVO occurred in 7 patients at the M2 segment, 4 patients at the M3 segment, 4 patients at the A2 segment, and 1 patient at the A3 segment.
Initially, primary occlusion treatment was conducted using Solitaire 4/20 in 5 patients, while Trevo 4/20 was used in 11 patients. These devices were consistently utilized for secondary lesions without switching the thrombectomy device. In 7 patients, the ACE 068 reperfusion catheter was employed as the first-line device without balloon guiding. Successful recanalization of the DVO was achieved in these cases using the Trevo 4/20 via the modified STR technique. Overall, complete recanalization of the primary occlusion was attained in 31.2% (5/16) of cases, classified as mTICI 2a, while 68.8% (11/16) of cases achieved mTICI 2b, taking into account the presence of DVO. The modified STR technique for secondary DVO yielded positive outcomes, with a low number of procedural runs (mean 1.5 times; range, 1–3) and successful recanalization (mTICI≥2c) in 93.8% (15/16) of cases, including a first-pass recanalization rate of 62.5% (10/16).
Regarding time metrics, the average duration from symptom onset to hospital admission was 78±46 minutes. The interval between symptom onset and femoral puncture for the procedure averaged at 124±54 minutes. The mean recanalization time was 65.6±12 minutes, with primary occlusion cases taking 47.5±15 minutes and secondary DVO cases taking 25.2±13 minutes (Table 2). During the removal of the secondary clot, 3 instances of vessel spasm and one case of dissection occurred, with no observed vascular perforation. The vessel spasms resolved spontaneously, but the dissection ultimately resulted in occlusion post-procedure. Asymptomatic ICH was detected in 6 patients on post-procedural CT scans, consisting of minor PH1 in four patients and subarachnoid hemorrhage in 2 patients. No neurological deterioration was observed in any of these cases.
Illustrative cases
Case 1. Patient 5
A 67-year-old woman presented with sudden-onset left-sided weakness and facial palsy with a NIHSS of 10. An initial CT showed an ASPECT score of 9 and multiphase CT angiography revealed a complete occlusion of the right ICA trunk with moderate collateral grade. IV tPA was administered but ineffective. After IV continuous sedation, 9 Fr balloon guide catheter was immediately placed at the proximal ICA and 5max reperfusion catheter was successfully achieved the recanalization of the distal ICA occlusion (Fig. 2A). However, one migrated embolus occurred at the right superior trunk of M3 (Fig. 2B). Immediately, Trevo XP Provue 4×20 mm was navigated to the DVO and the modified STR technique was successfully applied to the migrated embolus with a full restoration of the blood flow as mTICI3 (Fig. 2C, 2D). One day later, MRI showed a minor infarction on the internal capsule (Fig. 2E). At 3 months, the patient had a mild left-side weakness and a mRS score of 1.

(A) Initial angiography revealed a complete occlusion of the right internal carotid artery trunk (circle) with moderate collateral grade. (B) One migrated embolus (arrow) occurred at the right superior trunk of M3. (C) A Trevo XP Provue (4×20 mm) was navigated and the modified stent retrieval technique was applied to the migrated embolus. (D) Full restoration of the blood flow (mTICI 3) was seen. (E) One day later, magnetic resonance imaging showed a minor infarction on the right internal capsule.
Discussion
The elderly population inherently presents disadvantages such as small caliber, fragility, and tortuous anatomy of the affected vessels. In the case of distal emboli, the challenges mentioned above are further amplified. However, most of these studies have revealed that age alone is not a determining factor whether to treat the lesion with MT or not [2]. Therefore, it can be stated that excluding MT solely based on advanced age is not justified. Some studies have suggested that non-treated distal occlusions could progress into significant ischemic areas. Interestingly, recent reports have demonstrated favorable outcomes with a higher reperfusion rate in DVO, such as M2–3, A2–3, and P2–3 [8]. Consequently, these reports showed clinical improvement by achieving better quality mTICI scores through effective treatment of DVO. Therefore, MT for DVO should be actively considered even in the elderly population.
The modified STR technique employed in this study proved to be a valuable approach to manage secondary DVOs. Conceptually, secondary DVOs differ from primary DVOs [9] and often present with more severe clinical symptoms, larger extent of ischemia, and higher clot fragility. Nonetheless, the MT demonstrated favorable results with a high rate of successful reperfusion (mTICI≥2b) in 82% of cases and a low symptomatic ICH rate of 6%. These findings align with a meta-analysis by Rodriguez-Calienes et al. [9], which reported a successful reperfusion rate of 82% in patients with secondary DVOs treated with MT. The modified STR technique’s main principle is to reduce frictional force between the stent and the parent artery, minimizing the risk of vascular injury during the procedure. The use of stents suitable for distal vessels, such as Trevo Provue 4×20 mm and Solitaire Platinum 4×20 mm, proved effective in achieving clot entrapment and successful recanalization of DVOs [10].
It offers advantages in terms of time management and cost efficiency to manage elderly patients with acute LVO. The initial stent used for the primary occlusion can be continuously used for the migrated clot, eliminating the need to prepare a new device and saving time. Some devices suitable for DVO have demonstrated reliable performance based on angiographic and clinical results. The average procedural time reported for mini-stents was 45 to 50 minutes, and for aspiration catheters designed with a small diameter, it was 20 to 30 minutes for primary occlusions. When the guiding system was initially placed for reperfusion of the primary occlusion, mini-stents took 30 minutes and aspiration catheters took less than 30 minutes for secondary occlusions caused by migration. These differences are naturally influenced by device preparation. In this context, the average procedure time for the modified STR technique was 25.2±13 minutes, indicating a shorter duration compared to previous results targeting distal occlusions. During the procedure, the primary stent used for LVO can also be accessed for recanalization of the DVO without requiring additional tools. This not only reduces the financial burden on patients but also serves as a solution in countries with limitations on device availability due to reimbursement policies.
The utilization of small profile stents and aspiration catheters, such as Baby Trevo, Catch Mini, several intermediate catheters and Pneumbra 3 or 4 Max, has yielded promising outcomes in terms of success recanalization rate and one-pass rate [8,10,11]. These devices have shown impressive effectiveness in achieving successful restoration of blood flow in DVOs. Studies have reported high success recanalization rates, often exceeding 80% or more, indicating the ability of these small profile stents to effectively reopen blocked blood vessels. Additionally, the one-pass rate, which refers to achieving successful recanalization with a single pass, has been reported to be noteworthy about 50~60% with these devices. When comparing the favorable results of these new small devices in the treatment of DVOs, our findings are highly comparable and even more impressive. In contrast to the outcomes reported with the new small devices, our study demonstrated a notably higher success rate of mTICI 2c-3 reperfusion, achieving it in 15 out of 16 patients (93.8%) at the final recanalization rates, including all secondary DVO. Additionally, our one-pass rate of 62.5% compared with the reported rates with the new small devices. However, further research and evaluation are necessary to validate these findings and fully explore the potential of the modified technique in improving patient outcomes in the management of DVO.
Based on the available data, the reported rates of complications associated with additional procedures for secondary DVO align with findings from previous thrombectomy investigations. Approximately 1.7% of procedure-related vascular injuries have been reported, and a post-procedural hemorrhagic tendency has been reported in 0.9% of cases [12]. In this study, the occurrence of vessel spasm and dissection was found to be less than 1%, and these complications were effectively managed without resulting in severe consequences. Additionally, severe hemorrhagic changes related to the procedure were also less than 1%, indicating a low risk of significant bleeding complications. The incidence of asymptomatic ICH was relatively low, and there were no instances of neurological deterioration observed in the patients. These findings support the notion that the modified STR procedure exhibits a generally safe profile with manageable complications and a favorable risk profile.
This study has some limitations. Firstly, it is a retrospective study, which may introduce selection bias and limit the generalizability of the findings. Secondly, the sample size is relatively small, which could impact the statistical power and precision of the results. Additionally, the study lacks a control group for comparison, making it difficult to assess the specific impact of the modified STR technique on outcomes.
Conclusion
The modified STR technique is a feasible and effective approach for managing ENT following MT in elderly patients with acute large intracranial artery occlusions in the anterior circulation.
Notes
No potential conflict of interest relevant to this article was reported.


