Treatment strategy for osteoporotic vertebral body fractures in the lumbar spine: a case report and literature review
Article information
Abstract
This report describes the successful treatment of an osteoporotic compression fracture. A 74-year-old woman presented with severe low back pain and left sciatica that had lasted for 6 weeks. Four week of conservative treatment was not effective. The patient was bedridden and had difficulty walking. A past history of osteoporosis was noted. Multilevel compression fractures, central stenosis, and spondylolisthesis with overt instability were evident in the preoperative images. Decompression and fusion surgery, vertebroplasty, and preoperative and postoperative teriparatide administration were planned. A severe endplate injury in the lower vertebral body was detected during interbody fusion surgery using an anterior approach. Additional screw insertion with posterolateral fusion was planned to prevent aggravation of cage subsidence. Postoperative magnetic resonance imaging, computed tomography (CT), and X-ray images revealed sufficient decompression, no cement leakage, and no nerve injury. On the first postoperative day, the patient reported that the left sciatica symptoms had improved. Satisfactory ambulation was observed at the outpatient department after 6 months. Fusion in progress was evident on follow-up CT and X-ray images. This case offers insights into possible treatment strategies for osteoporotic compression fractures with severe endplate injury, overt instability, and radiculopathy of the lower lumbar spine.
Introduction
Osteoporosis is also associated with compression fractures. These fractures can worsen, and lead to additional fractures or spinal deformities [1]. If multilevel osteoporotic compression fractures in the lumbar spine are accompanied by overt instability and radiculopathy, decompression and fusion surgery, and vertebroplasty (VP) can be planned after conservative treatment [2,3].
Complications associated with fusion surgery, including cage subsidence, instrumentation failure, and pseudarthrosis are widely recognized [4]. Cage subsidence is a common complication in lumbar lateral interbody fusion [5]. Many risk factors for subsidence have been reported, including osteoporosis and endplate injury [6–8]. In particular, endplate injury is frequently associated with osteoporotic compression fractures [9].
Preventative measures to reduce the risk of cage subsidence are important for patients with osteoporotic compression fractures and severe endplate injuries who require fusion surgery. In this report, we describe the management of a patient with osteoporotic compression fractures with severe endplate injury, overt instability, and radiculopathy in the lower lumbar spine.
Case Report
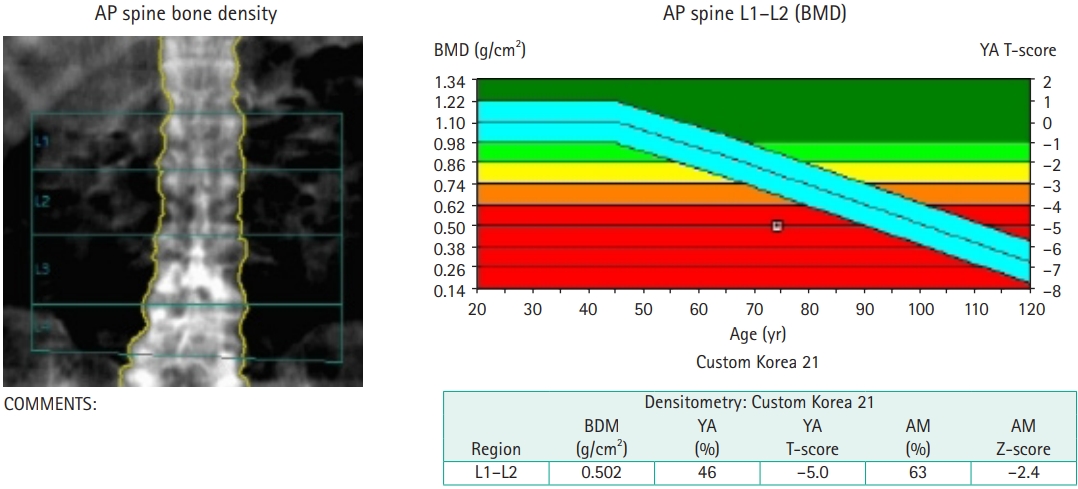
In March 2022, a 74-year-old woman presented to our hospital with a 6-week history of severe low back pain and left sciatica. Past history of osteoporosis was noted (bone mineral density [BMD] at the lumbar spine=–5.0) (Fig. 1). The patient had undergone conservative treatment for 4 weeks; however, this was not effective. She had difficulty walking and was bedridden because of pain. The patient’s numerical rating scale (NRS) score for pain was 8. Preoperative magnetic resonance imaging (MRI), computed tomography (CT), and X-rays revealed multilevel involvement of the spine including subacute compression fractures between L3 and L4, an acute compression fracture at L5, central stenosis with spondylolisthesis at L3–4 and L4–5 and instability at the L4–5 level (Fig. 2). Preoperative MR myelography showed signal blocks at the L3–4 and L4–5 levels (Fig. 2).
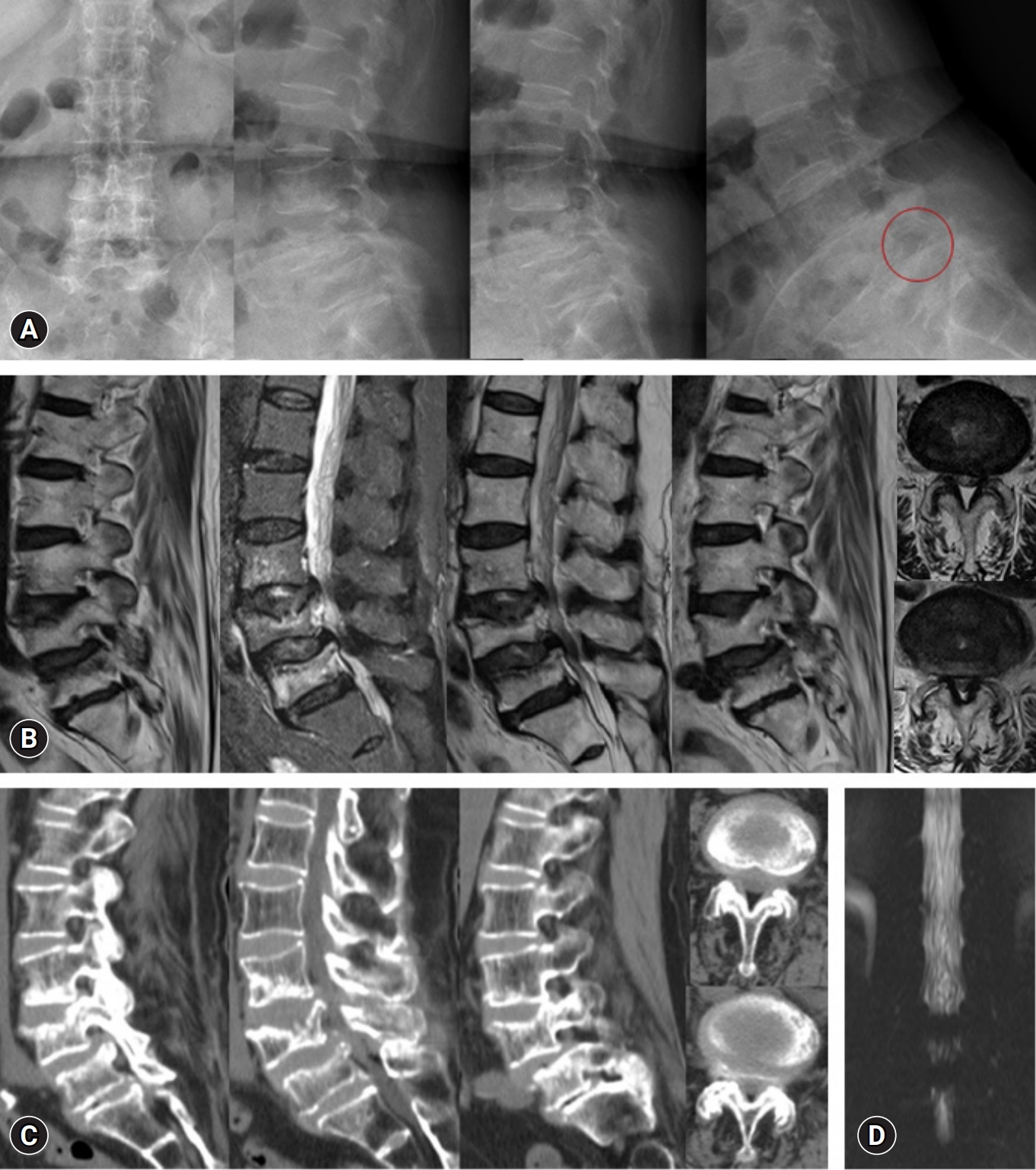
Preoperative images on X-rays, magnetic resonance imaging (MRI), computed tomography (CT), and magnetic resonance (MR) myelography. (A) X-rays (circle: instability). (B) Sagittal and axial MRI. (C) Sagittal and axial CT images. (D) An image on MR myelography.
The proposed management included oblique lumbar interbody fusion (OLIF) with cement-augmented pedicle screw insertion at the L4–5 level, unilateral laminotomy for bilateral decompression at the left L3–4 and L4–5 levels, VP at the L3 level, and preoperative and postoperative teriparatide (recombinant human parathyroid hormone, PTH 1–34). After informed consent was obtained from the patient, we proceeded with OLIF and severe endplate injury was observed in the lower vertebral body. Aggravation of the cage subsidence was expected after the operation (Fig. 3). Subsequently, after obtaining informed consent from the patient’s guardian, additional cement-augmented pedicle screw insertion at the S1 level with posterolateral fusion was performed to minimize the risk of cage subsidence (Fig. 3).
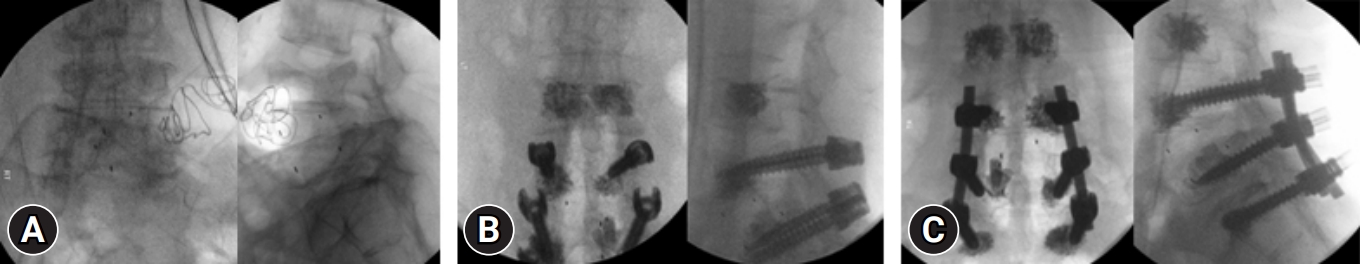
Intraoperative images. (A) Cage insertion. (B) Vertebroplasty at L3 and cement-augmented screw insertion at L4 and L5. (C) Additional S1 screw insertion with cement augmentation and posterolateral fusion.
Postoperative MRI, CT, and X-rays revealed sufficient decompression, no cement leakage, and no nerve injury (Fig. 4). On the first postoperative day (POD), the patient reported improved left sciatica symptoms (NRS score decreased from 8 to 3). The patient remained in bed until POD 14. On POD 15, the patient was allowed to sit with a brace while eating. On POD 25, the patient began walking with brace support. The patient was discharged on POD 30. At the outpatient department follow-up after 6 months, the patient was well ambulated. Progress in fusion was observed on follow-up X-rays and CT, without halo signs (Fig. 5).
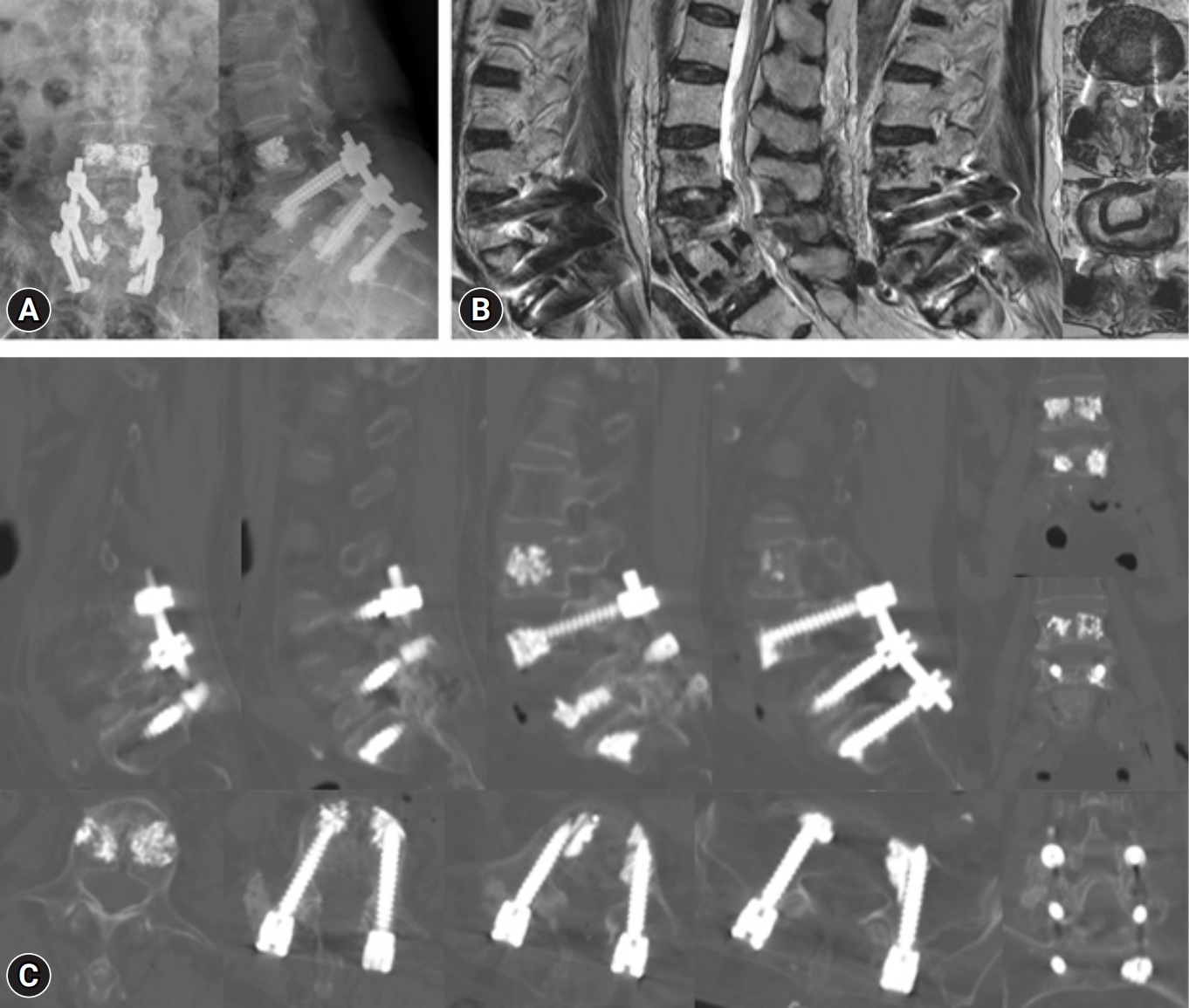
Postoperative images. (A) X-ray. Circle indicates instability. (B) Sagittal and axial magnetic resonance imaging. (C) Sagittal, axial, and coronal images on computed tomography.
Discussion
Compression fractures usually occur at the mid-thoracic spine (T7–8) and thoracolumbar junction (T12–L1) [10]. Multiple compression fractures occur in approximately 20 to 30 percent, and multilevel fractures occur in 1 to 5 continuous vertebral bodies. Spinal deformity is a common complication of compression fractures. Low BMD is significantly associated with vertebral deformities, including loss of mid-vertebral height. Together with old age, these factors predicted greater vertebral collapse and kyphoscoliotic deformities [1].
Conservative treatment alleviates back pain and functional disability [11]. However, long periods of immobilization and bed rest can lead to bone and muscle loss and adverse effects on cardiac and pulmonary functions in geriatric patients [12]. After conservative treatment, VP can be planned for continuous severe low back pain [13], and decompression and fusion surgery can be devised for overt instability and sciatica to improve clinical outcomes and reduce hospital stays [2,3].
Osteoporosis is a risk factor for complications of following fusion surgery including cage subsidence, instrumentation failure, and pseudoarthrosis [6,7,14]. Osteoporotic compression fractures are commonly accompanied by endplate injury [9] and endplate injury is a risk factor for cage subsidence following fusion surgery [8]. Strategies to prevent or minimize cage subsidence are necessary in a patient with osteoporotic compression fractures and severe endplate injuries.
Teriparatide is an anabolic agent approved by the US Food and Drug Administration to enhance bone formation. Subcutaneous administration of teriparatide during lumbar fusion surgery effectively improved the fusion rate [15]. The application of cement-augmented pedicle screws for multilevel lumbar fusion may provide better stability and lesser screw loosening than conventional pedicle screw fixation. The selective use of cement-augmented cranial and caudal screws may decrease the risk of complications associated with cement-augmented screw fixation [16].
After evaluating the preoperative images, osteoporotic compression fractures with endplate injuries at the interbody fusion level were confirmed. During interbody fusion using the anterior approach, severe endplate injury was observed macroscopically in the lower vertebral body. As a result, aggravation of cage subsidence was expected following fusion surgery. Consequently, additional cement-augmented pedicle screw insertion with posterolateral fusion was planned, and informed consent was obtained from the patient’s guardian.
Six months after surgery, the patient appeared well-ambulated at the outpatient follow-up department. Subsidence was not aggravated, and fusion was in progress on follow-up X-rays or CT, without halo signs.
If osteoporotic compression fractures present with endplate injury and radiculopathy but without overt instability after conservative treatment, only decompression or ligamentoplasty with cementoplasty may be considered to prevent cage subsidence after interbody fusion surgery.
Conclusion
This case offers insights into the possible treatment strategies for osteoporotic compression fractures with overt instability and radiculopathy of the lumbar spine.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.