Introduction
Decompression alone has been performed to treat degenerative lumbar spinal stenosis without instability for many years. In case of degenerative lumbar spinal stenosis with instability, fusion surgery has been the primary choice to prevent worsening of instability. However, there are borderline patients with mildly unstable degenerative lumbar spinal stenosis. Ligamentoplasty can fill a gap between decompression alone and fusion in the spectrum of surgical treatment for degenerative lumbar spinal stenosis, and many studies supported that ligamentoplasty represents a viable option for patients who have significant comorbidities or are elderly [
1-
3].
Fusion surgery needs additional blood loss and tissue stripping, and this method inevitably increases the risk of damage at the adjacent structure and perioperative complications, including cage subsidence, screw failure, non-union, and so on [
4]. Comparatively, ligamentoplasty can decrease perioperative complications, because it can reduce incision and injury to surrounding tissues. Furthermore, it can lessen the possibility of fusion surgery due to lumbar instability after surgery [
5]. In this report, we present 2 patients with lumbar spinal stenosis that coexists with mild segmental instability and vertebral body fracture, who were successfully managed with interspinous ligamentoplasty.
Instability
When flexion and extension X-ray in the sagittal plane show 10 degrees angular motion or more, or 4 mm translation or longer, instability can be defined [
6]. And fusion surgery can be considered. In case of 10 degrees angular motion or less, or 4mm translation or shorter in dynamic X-ray, minimal or mild instability can be decided [
2]. Fusion surgery in traumatic thoracolumbar fractures (T10-L2) can be also chosen in case of 4 points or more in the modified thoracolumbar injury classification and severity score (TLICS) system using magnetic resonance imaging (MRI) and computed tomography (CT) images [
7].
Case Report
Case 1
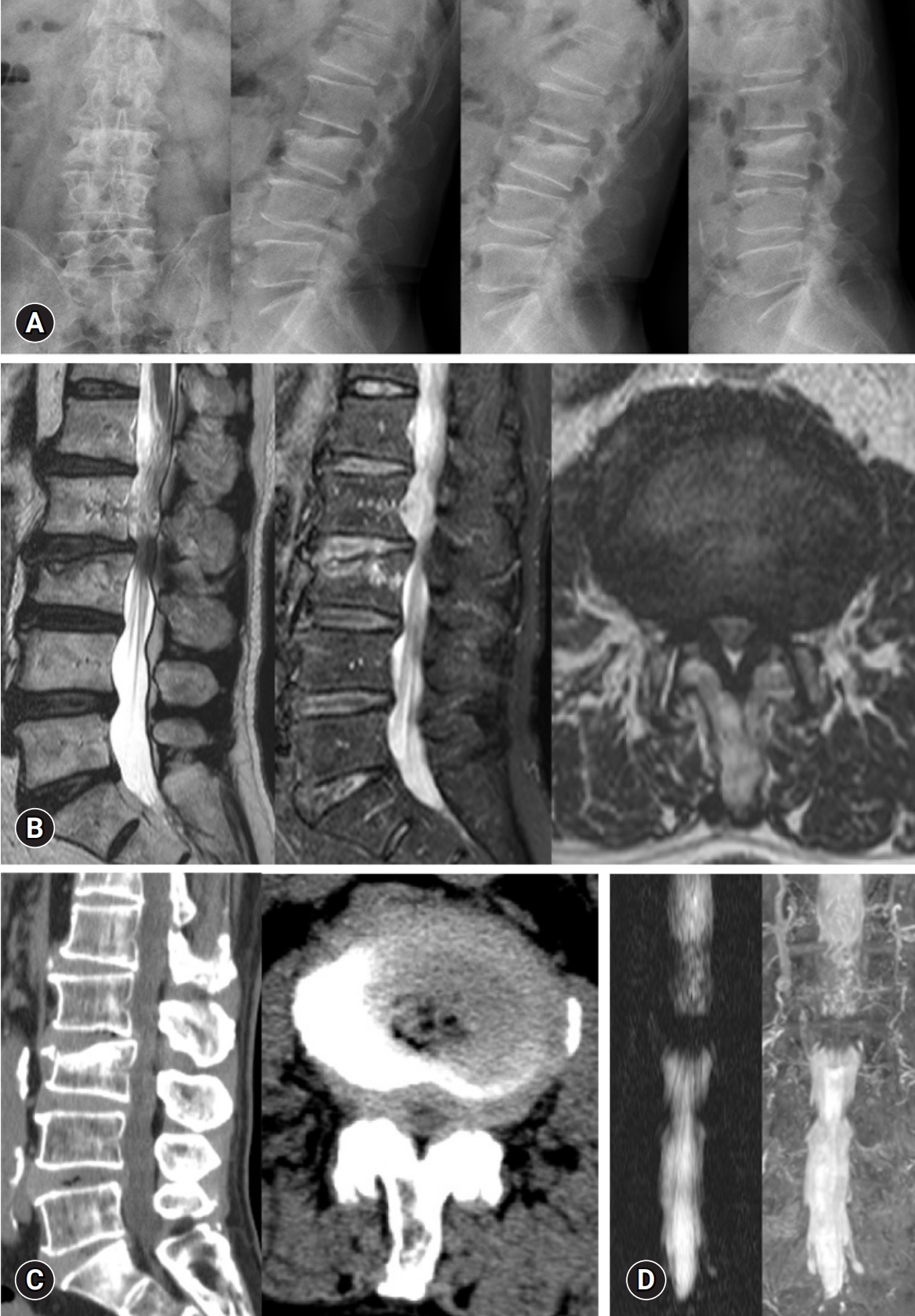
A 74-year-old woman presented to our hospital in April 2022, with a two-month history of right sciatica. The pain as assessed by the numeric rating scale (NRS) leg was 8. The patient also complained of continuous back pain (NRS back=7) regardless of 4 weeks of conservative treatment after slip down. Past history included osteoporosis (bone mineral density at lumbar spine=-2.5 standard deviation). Preoperative MRI, CT, and plain X-ray revealed central stenosis with grade 1 degenerative spondylolisthesis at the L4-5 level and acute compression fracture at L4 level (
Fig. 1). The preoperative flexion and extension X-ray demonstrated slippage and instability. Interspinous ligamentoplasty using the sagittal horizontal ligament (SHL, Ligament Vertebralde Renfort; Cousin Biotech) at the L4-5 level and vertebroplasty (VP) at L4 were performed after obtaining informed consent from the patient. On the first postoperative day (POD), right sciatica and back pain improved to 4 on the NRS leg and back scores. The patient was discharged on the eleventh POD and the pain improved to 3 on the NRS back and leg scores. On the outpatient department (OPD) follow-up after 1 month and 1 year, improved state remained.
Case 2
A 74-year-old man presented to our hospital in April 2022, with a two-month history of bilateral sciatica. The patientŌĆÖs pain scored 8 on the NRS leg. He also had accompanying back pain (NRS back=8). Preoperative MRI, CT, and plain X-ray revealed central stenosis with grade 1 degenerative spondylolisthesis at the L2-3 level and subacute compression fracture at L3 level, and the preoperative flexion and extension X-ray demonstrated minimal instability, because he canŌĆÖt make flexion and extension well due to severe back pain (
Fig. 2). Interspinous ligamentoplasty with the SHL at the L2-3 level was performed after obtaining informed consent from the patient. On the first POD, bilateral sciatica and back pain improved to 4 on the NRS back and leg scores. The patient was discharged on the tenth POD and the pain improved to 3 on the NRS back and leg scores. On the OPD follow-up after one month, the pain improved to about 90 percent. On the OPD follow-up after 1 year, segmental instability was not aggravated.
Technical notes
The patient is placed in the prone position under general anesthesia. A midline skin incision was made at the relevant level. Bilateral partial laminotomy with foraminotomy and medial facetectomy was done with a drill and all thickened ligamentum flava including foraminal extension were completely removed under microscopic view. Spinous process and supraspinous ligament were preserved at the target level. The artificial ligament (SHL) was soaked in saline containing antibiotics and povidone-iodine solution. After checking for sufficient decompression and removing the bony spikes and remnant ligamentum flavum, the spine position was changed from flexion to extension to form a lordotic curvature. Initially, the upper and lower spinous processes were wrapped with the sagittal ligament of the SHL in a figure-eleven pattern (
Fig. 3A). The horizontal ligament of SHL was tightly tied near the center of the sagittal ligament to replace the interspinous ligament and stabilize the target level with sutures (
Fig. 3B). The artificial ligaments were fixed to position using a non-absorbable suture.
Discussion
Degenerative lumbar spinal stenosis, a common disease for elderly patients, has been treated with decompression alone to relieve neural component. Additional spinal stabilization may improve the surgical outcomes and fusion surgery is the most widely accepted stabilization method. Moreover, in the thoracolumbar vertebral fracture, fusion surgery can be chosen in case of 4 points or more in the modified TLICS system [
7]. However, for some patients with mild segmental instability, fusion methods are more invasive. Soft stabilization methods have been introduced to fill a gap between fusion and only decompression in the spectrum of surgical treatment for degenerative spinal stenosis, including ligamentoplasty [
8,
9].
Ligamentoplasty canŌĆÖt be a full replacement for fusion surgery, because no hard interspinous anchoring canŌĆÖt be strong enough to correct advanced spondylolisthesis. A potential complication of the ligamentoplasty is fractures of spinous processes. This is particularly relevant to elderly women with osteoporosis, but this complication was not observed in previous study [
2]. However, the artificial ligament can give support to the existing structures. And the development of a fibrous fusion can also provide structural support and prevent postoperative instability after decompression and progressive spondylolisthesis [
9,
10]. Ligamentoplasty can also be a feasible option for patients who are elderly or have significant comorbidities [
3].
Many studies reported that VP for acute vertebral compression fracture (Ōēż6 weeks), particularly in patients with severe pain, was superior to conservative treatment [
11]. Delayed VP did not lessen the operation ratio compared to early VP. This delayed strategy may also lead unnecessary delay of treatment for patients who want rapid pain relief and spend more medical expenses for hospitalization and conservative treatment. Furthermore, in the current study, cement leakage and interdigitation were significantly favorable in the patient group with early VP compared with delayed VP group [
12].
Our 2 patients had compression fractures. After applying interspinous ligamentoplasty to the relevant level, the patientsŌĆÖ symptoms improved and postoperative MRI demonstrated sufficient decompression (
Figs. 4,
5). These patients were prevented from postoperative complications after fusion surgery, including aggravation of cage subsidence, because vertebral body fractures in the relevant level increase the progression of cage subsidence. At the time of discharge, the back pain and sciatica were improved to an NRS score of 3. Further improvements of symptoms were observed during the outpatient follow-ups.
Conclusion
Interspinous ligamentoplasty can be a good surgical option for lumbar spinal stenosis that coexists with mild segmental instability and vertebral body fracture.













 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



