Efficacy of the five-item modified frailty index for predicting a poor prognosis in patients undergoing posterior lumbar interbody fusion surgery for lumbar spinal stenosis
Article information
Abstract
Objective
This study aimed to determine whether preoperative frailty assessed using the five-item modified frailty index (mFI-5) in patients undergoing posterior lumbar interbody fusion for lumbar spinal stenosis can predict poor patient outcomes.
Methods
We retrospectively included 192 patients aged 18 years or older who were diagnosed with lumbar spinal stenosis and underwent posterior lumbar interbody fusion at a single hospital between March 2009 and February 2021. We calculated mFI-5 scores for these patients based on the following five comorbidities: (1) hypertension requiring medication, (2) diabetes mellitus, (3) history of chronic obstructive pulmonary disease or pneumonia, (4) history of congestive heart failure in the 30 days before surgery, and (5) partially or totally dependent functional health status at the time of surgery. The patients were categorized into three groups according to their mFI-5 scores, and these groups were analyzed. A P<0.05 was considered statistically significant in all analyses.
Results
Length of hospital stay (LOS) was significantly associated with mFI-5 score (β=0.196, P=0.008), age (β=0.112, P=0.159), and surgical level (β=0.238, P<0.001). In patients with fusion at one or two levels, mFI-5 score showed the greatest association with LOS (β=0.188, P=0.016), followed by sex (β=0.137, P=0.065) and the number of fused segments (β=0.137, P=0.065).
Conclusion
Frailty may not be an independent predictor, but it has significant predictive power for LOS in patients undergoing posterior lumbar interbody fusion for lumbar spinal stenosis, especially in patients undergoing fusion at one or two levels.
Introduction
Patients with low back pain due to degenerative lumbar spinal disease, including lumbar spinal stenosis, account for the largest proportion of people with a single disability worldwide [1,2]. Posterior lumbar interbody fusion is a good treatment option for degenerative lumbar spinal stenosis [3–5]. With aging, the cost burden of degenerative lumbar spinal stenosis gradually increases. Efforts are being made to reduce costs without compromising the quality of patient care. As part of that effort, it is important to effectively predict poor prognosis and appropriately select patients for surgical treatment [6].
A prolonged length of hospital stay (LOS) and unplanned readmission are common indicators of poor prognosis. These indicators are associated with the outcomes of medical and surgical procedures, including poor prognosis owing to various complications, mortality, and increased medical cost in patients undergoing spine surgery [7–9]. A prolonged LOS has been associated with reoperation and perioperative complications in patients who underwent posterior lumbar interbody fusion for degenerative spinal diseases [10]. Therefore, efforts are being made to identify patient-related risk factors for a prolonged LOS, unplanned readmission within 30 days of discharge, and reoperation [11].
Frailty, a multifactorial concept, is related to aging. It denotes that a person’s energy metabolism, strength, endurance, and functional level are lower than what can be expected considering their age group [12–15]. Frailty is highly associated with a poor prognosis after surgery [16]. It is also independently associated with poor prognoses, such as a prolonged LOS and increased complication rates, in patients undergoing spine surgery [17–21].
The modified frailty index was proposed and developed by the American College of Surgeons National Surgical Quality Improvement Program. Initially, an 11-item frailty index (mFI-11) was developed, which was revised to develop the five-item modified frailty index (mFI-5) in 2012. Several studies have shown that the mFI-5 has comparable prognostic potential to the mFI-11 [22,23]. The mFI-5 incorporates the following five comorbidities: hypertension requiring medication, diabetes mellitus, history of chronic obstructive pulmonary disease, congestive heart failure in the 30 days before surgery, and partially or totally dependent functional health status at the time of surgery. The mFI-5 score has been found to be associated with poor prognosis after surgery in various fields [24–26].
As the average age of patients undergoing spine surgery increases, the rate of frailty in them will also increase. Therefore, it is important to know how preoperative frailty affects prognosis to enable the appropriate selection of patients for surgery. However, there are few studies on the association between frailty and poor prognosis in patients with lumbar spinal stenosis.
The purpose of this study was to determine whether preoperative frailty assessed using the mFI-5 in patients undergoing posterior lumbar interbody fusion for lumbar spinal stenosis could predict poor patient outcomes.
Material and Method
Patient selection
The present study protocol was approved by the Institutional Review Board of Inje University Sanggye Paik Hospital (IRB No.2022-06-002). We retrospectively included 192 patients aged 18 years or older who were diagnosed with lumbar spinal stenosis and underwent posterior lumbar interbody fusion at a single hospital between March 2009 and February 2021. Patients were enrolled based on the International Classification of Diseases codes. The exclusion criteria were history of spine surgery, pregnancy, ventilator dependence, preoperative sepsis, disseminated cancer, and LOS longer than 1 year.
Data collection
Preoperative patient factors including age, sex, body mass index (BMI), comorbidities, functional health status at the time of admission and surgery, and medical history were recorded. The number of fused segments was evaluated as an operative factor. Postoperative factors including LOS, postoperative complications, unplanned readmission within 30 days of discharge, and reoperation were also recorded and assessed.
Calculation of the mFI-5 score
We calculated mFI-5 scores for all the patients based on the following five comorbidities: (1) hypertension requiring medication, (2) diabetes mellitus, (3) history of chronic obstructive pulmonary disease or pneumonia, (4) history of congestive heart failure in the 30 days before surgery, and (5) partially or totally dependent functional health status at the time of surgery. One point was assigned to each factor, and the total score ranged from 0 to 5. Based on previous literature, patients were divided into three groups according to their mFI-5 scores for analysis and comparison: (1) “not frail (mFI-5=0)”, (2) “pre-frail (mFI-5=1)”, or (3) “frail (mFI-5>1)” [27].
Statistical analysis
The statistical analyses were performed using IBM SPSS for MAC ver. 25.0 (IBM Corp., Armonk, NY, USA). The differences of three groups according to mFI-5 scores were analyzed. A P-value of <0.05 was considered statistically significant in all analyses. Descriptive statistical analysis, Pearson correlation analysis, and univariate and multivariate linear regression analyses were performed. To exclude the effect of the number of fused segments, we performed the univariate and multivariate analysis only for patients with one or two fused segment levels. Analysis of variance with Scheffé test was used to compare normally distributed variables and the Kruskal–Wallis H test and Mann–Whitney U test were used to compare non-normally distributed variables among the three groups.
Results
Patient demographics
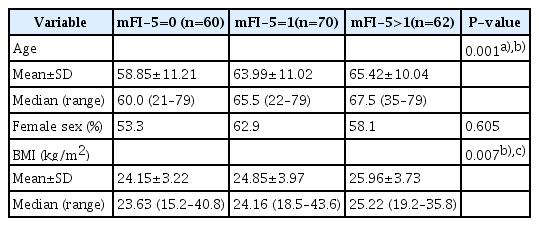
Of the 192 patients included, 60 (31.3%), 70 (36.5%), and 62 (32.3%) were categorized into the mFI-5=0, mFI-5=1, and mFI-5>1 groups, respectively. The mFI-5>1 group was older (65.4 years vs. mFI-5=1: 64 years and mFI-5=0: 58.9 years, P=0.001) and had greater BMI (26 kg/m2 vs. mFI-5=1: 24.9 kg/m2 and mFI-5=0: 24.2 kg/m2, P=0.007) than the other groups. There was no significant correlation between the sex composition ratio between each group (Table 1).
Patient comorbidities
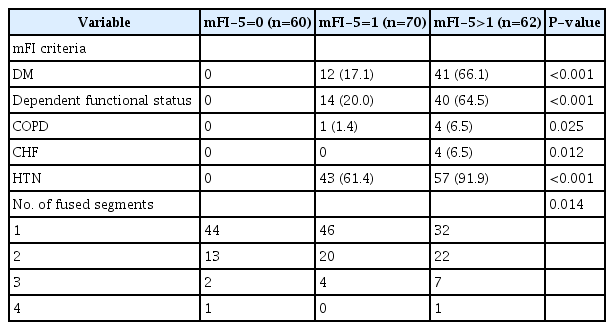
The most common comorbidity with respect to the mFI-5 items was hypertension (mFI-5=1: 61.4% and mFI-5>1: 91.9%). Other factors, including diabetes and dependent functional status, were also more common in the mFI-5>1 group than in the mFI-5=1 group (Table 2).
LOS and 30-day readmission and reoperation rates
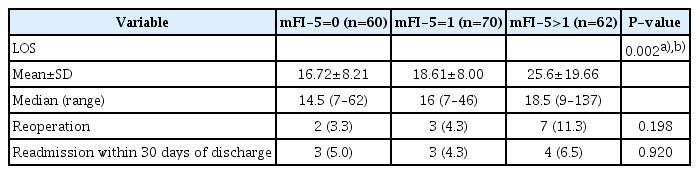
The LOS was longer in the mFI-5>1 group than in the other groups (25.6±19.7 days vs. mFI-5=1: 18.6±8.0 days and mFI-5=0: 16.7±8.2 days, P=0.002). The mFI-5>1 group showed a greater reoperation rate than the other groups (11.3% vs. mFI-5=1: 4.3% and mFI-5=0: 3.3%, P=0.006), but there was no significant difference in readmission rate among the groups (Table 3).
Univariate and multivariate linear regression analysis for LOS
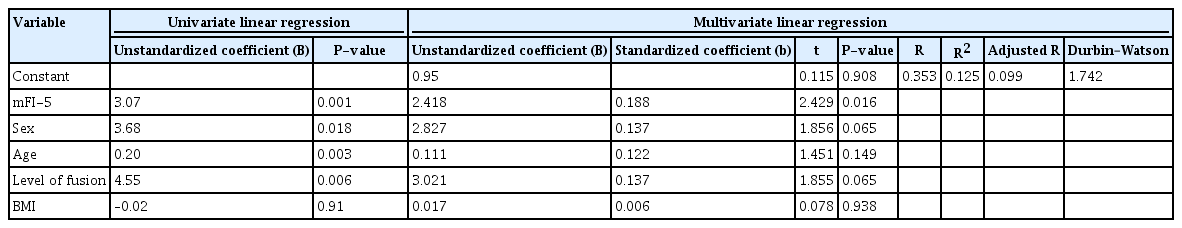
In the univariate and multivariate linear regression analysis, LOS was significantly associated with mFI-5 score (β=0.196, P=0.008), age (β=0.112, P=0.159), and surgical level (β=0.238, P<0.001) (Table 4). In the univariate and multivariate linear regression analysis conducted only on patients with 1 or 2 fused segments, the mFI-5 score showed the greatest association with LOS (β=0.188, P=0.016), followed by sex (β=0.137, P=0.065) and the number of fused segments (β=0.137, P=0.065) (Table 5).
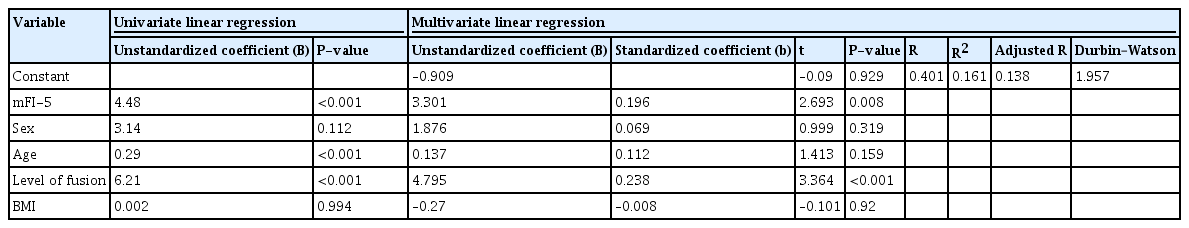
Univariate and multivariate linear regression analysis of the associations of preoperative variables with the length of hospital stay
Discussion
With aging, the morbidity of degenerative lumbar spine disease and requirement of spine surgery increase. By analyzing the preoperative frailty and surgical risk factors of patients with degenerative lumbar spine disease, it is possible to minimize postoperative complications and reduce unnecessary medical expenses. Several indices have been proposed for evaluating frailty, and we used the mFI-5 in this study. The association of mFI-5 with the prognosis of orthopedic surgery has been studied. Segal et al. found that high mFI-5 scores were associated with increased rates of adverse events, life-threatening complications, readmission within 30 days of discharge, and adverse discharge disposition in patients who underwent kyphoplasty for vertebral augmentation [28]. Similarly, Wilson et al. found that high mFI-5 scores were associated with increased rates of reoperation within 30 days of surgery, readmission, and complications in patients with distal radius fractures who underwent surgery [29]. Frailty has been found to be associated with a prolonged LOS and increased rates of complications in patients who underwent spine surgery [17–21], and a similar association was found in our study, which included patients who underwent posterior lumbar interbody fusion for lumbar spinal stenosis. Spine surgeons may be able to preoperatively distinguish high-risk patients who are likely to have a poor prognosis after surgery and those who can expect good recovery after surgery by analyzing frailty-related factors.
In studies on the prognosis of patients undergoing spine surgery, the proportion of patients classified as “frail” based on their mFI-5 scores ranges from 1.3% to 20% [30,31]. This wide distribution reveals that there is a unique subpopulation. However, the cause of the discrepancy is unclear, suggesting that further research on patients undergoing posterior lumbar interbody fusion is needed [32].
An analysis of our entire study cohort revealed that a high mFI-5 score was associated with an increased LOS and high reoperation rate, but the mFI-5 score could not be regarded as an independent predictor of a prolonged LOS. Known poor prognostic factors, such as age, BMI, and surgical level, were found to have a large impact on increased LOS. To exclude the effect of surgical factors, the multivariate linear regression analysis was performed only in patients who had undergone fusion at one or two levels, and the mFI-5 score was confirmed as the most powerful factor predicting LOS.
Obesity is associated with poor prognosis after surgery in patients with degenerative lumbar diseases [33,34]. However, we found that BMI had statistically no correlation with increased LOS. This is thought to be because our study included patients with lumbar spinal stenosis who underwent posterior lumbar interbody fusion. In patients with high BMI, less invasive surgical techniques are associated with a good recovery and prognosis after surgery. Since posterior lumbar interbody fusion is more complex than other surgical techniques such as microscopic discectomy or decompressive posterior laminectomy, patients with high BMI are not priority candidates for posterior lumbar interbody fusion.
In our study, the reoperation rate tended to increase with an increase in the mFI-5 score but was not statistically significant. The statistically insignificant results might have been because the total number of patients in our study was not large, so the number of patients who underwent revision surgery was not large enough for meaningful analysis. Additional studies with a larger number of patients will help to elucidate the relationship between mFI-5 and reoperation rate.
There are several limitations to this study. One of them is the retrospective design of the study. Additionally, the study included patients who underwent surgery at a single hospital; therefore, there may be selection bias. Since the patients were enrolled based on International Classification of Diseases codes, there may be coding and reporting bias as well as a possibility of misclassified or incomplete data. In this study, the proportion of patients categorized as “pre-frail” or “frail” was relatively high (68%), which is thought to be the result of including patients with a relatively high severity of lumbar spinal stenosis that required surgical treatment. Therefore, it is difficult to generalize the results of this study to the entire population. Furthermore, the average age of the frail group tended to be higher than that of the other groups, and this suggests that there may confounding factors. In this study, operative factors such as case complexity were not considered. Furthermore, certain complications of spinal fusion surgery, such as radiographic evidence of adjacent segment disease or postoperative neurological deficit, were not analyzed [35,36]. Although this study confirmed the association between mFI-5 score and poor prognosis after surgery, other conditions can also predict poor prognosis after posterior lumbar interbody fusion. Spine-specific preoperative patient conditions such as symptom duration and the severity of leg and back pain have been found to be associated with a poor prognosis in elective lumbar spine surgery [37]. Prospective studies using the mFI-5 and further research to develop a frailty index that can be used to predict the prognosis after spine surgery are needed.
Conclusion
Our study shows that frailty is not an independent predictor but can be considered a valuable predictive factor for LOS in patients undergoing posterior lumbar interbody fusion for lumbar spinal stenosis. Additionally, frailty can be considered an independent predictor of poor prognosis in patients undergoing fusion at one or two levels. The presence of frailty should not be a contraindication for surgical management in patients with spinal stenosis; however, in combination with other comorbidities, it may aid risk stratification in patients undergoing spine surgery.
Notes
No potential conflict of interest relevant to this article was reported.