1. Rubin MP, Chechurin RE, Zubova OM. Osteoporosis: diagnosis, current approaches to treatment, prophylaxis. Ter Arkh 2002;74:32-7.
2. Kim SS, Lee DH, Kim JH, et al. Risk Factors for subsequent vertebral compression fracture following osteoporotic compression fracture. J Korean Orthop Assoc 2016;51:479-85.


3. Crans GG, Silverman SL, Genant HK, Glass EV, Krege JH. Association of severe vertebral fractures with reduced quality of life: reduction in the incidence of severe vertebral fractures by teriparatide. Arthritis Rheum 2004;50:4028-34.


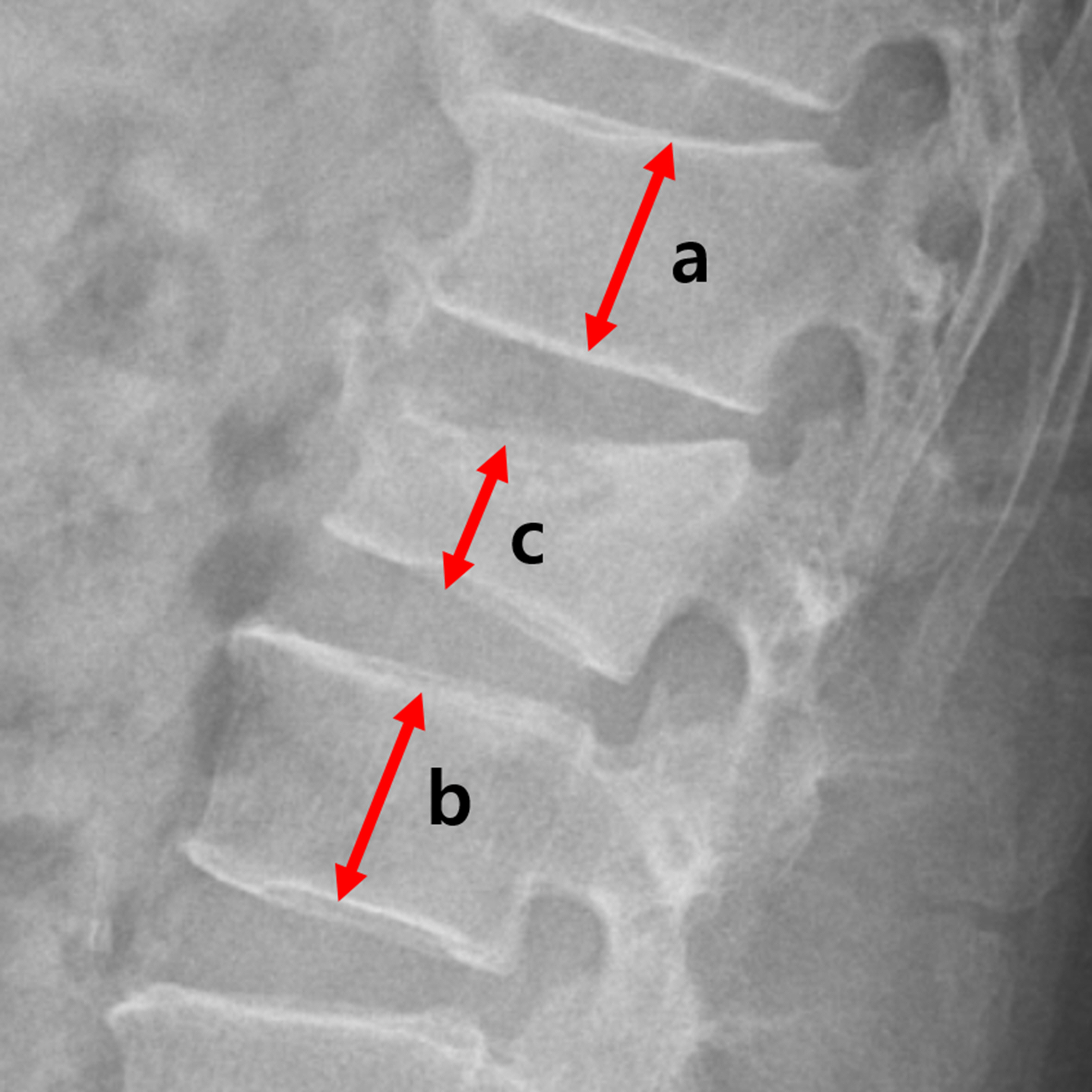
6. Goldstein S, Smorgick Y, Mirovsky Y, Anekstein Y, Blecher R, Tal S. Clinical and radiological factors affecting progressive collapse of acute osteoporotic compression spinal fractures. J Clin Neurosci 2016;31:122-6.


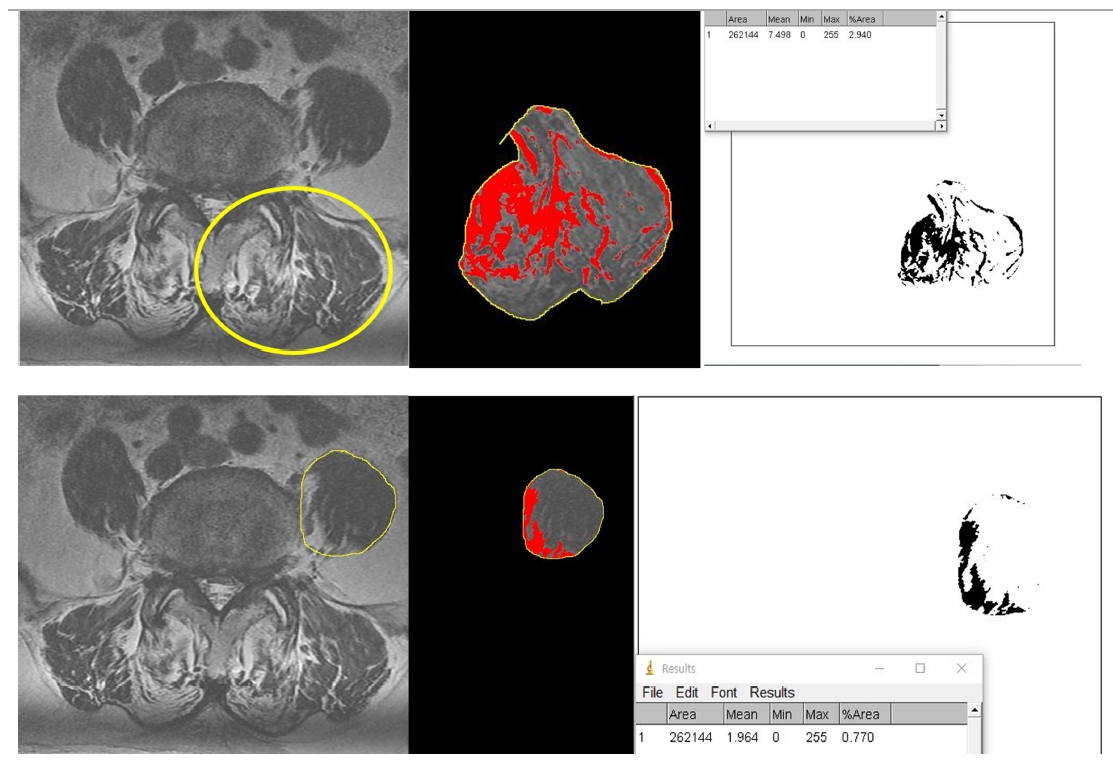
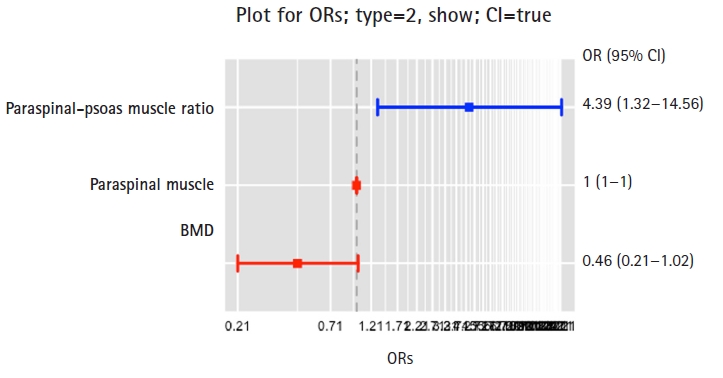
8. Jeon I, Kim SW, Yu D. Paraspinal muscle fatty degeneration as a predictor of progressive vertebral collapse in osteoporotic vertebral compression fractures. Spine J 2022;22:313-20.


10. Du Y, Karvellas CJ, Baracos V, Williams DC, Khadaroo RG; Acute Care and Emergency Surgery (ACES) Group. Sarcopenia is a predictor of outcomes in very elderly patients undergoing emergency surgery. Surgery 2014;156:521-7.


11. Reisinger KW, van Vugt JL, Tegels JJ, et al. Functional compromise reflected by sarcopenia, frailty, and nutritional depletion predicts adverse postoperative outcome after colorectal cancer surgery. Ann Surg 2015;261:345-52.


13. Bayram S, Akg├╝l T, Ad─▒yaman AE, Karalar ┼×, D├Člen D, Aydoseli A. Effect of sarcopenia on mortality after percutaneous vertebral augmentation treatment for osteoporotic vertebral compression fractures in elderly patients: a retrospective cohort study. World Neurosurg 2020;138:e354-60.


14. Bokshan SL, Han AL, DePasse JM, et al. Effect of sarcopenia on postoperative morbidity and mortality after thoracolumbar spine surgery. Orthopedics 2016;39:e1159-64.


15. Jun HS, Kim JH, Ahn JH, et al. The effect of lumbar spinal muscle on spinal sagittal alignment: evaluating muscle quantity and quality. Neurosurgery 2016;79:847-55.


19. Crisco JJ 3rd, Panjabi MM. The intersegmental and multisegmental muscles of the lumbar spine: a biomechanical model comparing lateral stabilizing potential. Spine (Phila Pa 1976) 1991;16:793-9.


20. McGill SM, Grenier S, Kavcic N, Cholewicki J. Coordination of muscle activity to assure stability of the lumbar spine. J Electromyogr Kinesiol 2003;13:353-9.


21. Sanaka K, Hashimoto K, Kurosawa D, et al. The psoas major muscle is essential for bipedal walking: an analysis using a novel upright bipedal-walking android model. Gait Posture 2022;94:15-8.













 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



