Introduction
Posterior screwing with interbody fusion is commonly performed for the treatment of many different spine pathologies. Despite immediate and strong fixation, as well as a relatively few device-related complications, screw fixation for the purpose of bone fusion in the soteopenic or osteoporotic spine still remains a challenge [
1,
2]. A typical complication of pedicle screw fixation is screw loosening and the estimated rate ranges from 0.8% to 27%, and the incidence rate increases rapidly in cases of severe osteoporotic spine [
3,
4].
In cases of symptomatic pedicle screw loosening unfortunately, few treatment options exist. The typical treatment is extensive open surgery with hard ware revision such as extended fusion level and multisegmental screw fixation.
Recently, due to the reluctance of the surgeon for extensive revision surgery, minimally invasive cement augmentation using polymethylmethacrylate (PMMA) to treat cases of clinically relevant pedicle screw loosening has been reported [
5,
6]. However, as far as the authorsŌĆÖ knowledge, cement augmentation has not been proven as the definitive method of alleviating pain resulting from screw loosening. Moreover, screw loosening because of bone resorption around implants can be caused by spinal infections, which can be a contraindication for PMMA augmentation [
7].
The aim of this study was to assess the results of percutaneous reimplantation of pedicle screws via a different trajectory for clinically relevant screw loosening, which is usually requires extensive revision surgery with multisegmental screw fixation.
Material and Method
This study was approved by the Institutional Review Bord of Chosun University Hospital (IRB No: 2020-01-007-006) which waved the requirement for informed consent due to the respective nature of study.
We obtained and analyzed the records of 10 consecutive patients with symptomatic pedicle screw loosening who had undergone percutaneous reimplantation of screws from June 2015 to July 2018.
These patients had undergone previous single-level lumbar interbody fusion and percutaneous screw fixation for degenerative lumbar spine diseases, complicated by symptomatic pedicle screw loosening. The surgical inclusion criteria were as follows: (1) development of continuous para-midline back pain resistant to conservative treatments after posterior lumbar interbody fusion (PLIF) surgery; (2) typical finding of radiolucent halo zones around the screws at a vertebral level on both plain radiography and computed tomography (CT); and (3) screw loosening without a prominent screw back-out or strip which needed extensive open surgery. Patients with significant coagulopathy or prominent spondylitis with marked level of elevated infection markers at the time at previous lumbar interbody fusion were excluded.
Demographic data of the 10 patients were obtained and analyzed for their age, sex, preoperative diagnosis, bone mineral density, and modified MacNabŌĆÖs criteria at final follow-up (
Table 1). The patients underwent percutaneous reimplantation of screws via a different trajectory with larger-diameter screws. Follow-up was performed clinically and radiologically 1, 2, 3, 6 months after surgery and at final follow-up with a clinical visit and using standing plain radiographic films.
Surgical technique
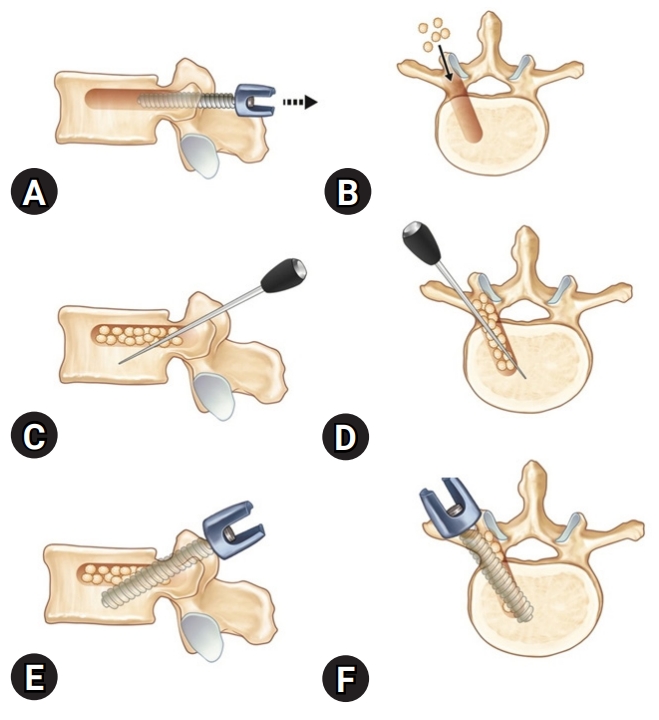
Under general anesthesia, the patient was placed in the prone position. A paraspinal longitudinal skin incision was made at the site of previous percutaneous screw fixation. Subsequently, the wound was dissected, and the loosened screws and rods were removed (
Fig. 1A), most of which did not require much effort. Soft tissues in the previous screw fixation site were dissected, and massive irrigation was performed. The tract was palpated with a straight probe to identify the pedicle wall; allograft bone chips were used to fill the tract of the removed screw to the maximum possible level (
Fig. 1B).
The new screw entry point was generally superior to the previous screw insertion site. The new trajectory was targeted to pass over the anterior three quarters of the vertebral body to the midline, crossing the course of the loosened screw at the level of the posterior wall and running obliquely from the lateral direction to the medial and cephalad directions and finally to the caudal direction (
Fig. 1C,
D). After guiding the new transpedicular screw to the new entry point, it was inserted following the new trajectory (
Fig. 1E,
F). If there was no evidence of screw loosening, allograft bone chips were used to fill the tract of the removed screw to the maximum possible level, and a new same-size screw was inserted following the previous trajectory. After we confirmed that the new screw, which had a larger diameter compared to the previous screw, was successfully inserted in place, the operative wound was closed in layers with Vicryl sutures using an auto-stapler (
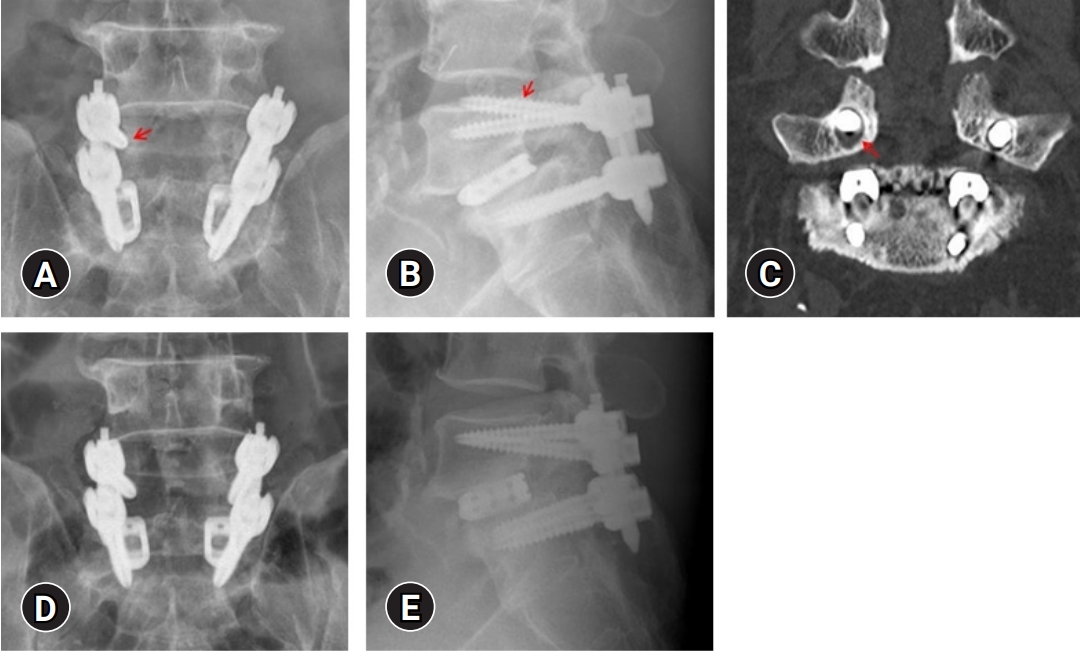
Figs. 2 and
3).
Safety and outcome measurement
Patients were evaluated during the follow-up period using the visual analogue scale (VAS) and with the modified MacNabŌĆÖs criteria for characterizing clinical outcomes of spinal surgery at the final follow-up. The paired t-test was used for comparisons at different time points, and differences were considered statistically significant at P<0.05.
Results
A total of 10 patients (7 males and 3 females) underwent percutaneous reimplantation of larger screws via a different trajectory. All patients had newly developed back pain after a period of pain relief, and the mean revision time was 9.9 months from previous PLIF surgery.
The mean age of the patients was 66.1 years (range, 58-76 years), and the mean follow-up period was 11.2 months (range, 6-14 months).
Table 1 presents the demographics of all study participants. All patients had osteopenia or osteoporosis. Screws could be inserted via a new trajectory in all patients.
At the final follow-up after the revision surgery, nine patients (90%) showed excellent or good outcomes based on the modified MacNabŌĆÖs criteria. Before revision surgery, the mean pain score on VAS was 6.9, which decreased to 3.1 at the final follow-up (P<0.05). No loosened or stripped screws were observed in any study participant, and no patient required extensive open surgery.
Discussion
Pedicle screw fixation is an essential technique for spinal fusion surgery. It is widely used, because it provides immediate and strong fixation. However, it often results in complications and symptomatic screw loosening is one of these complications. Pedicle screw loosening is the main cause of morbidity in patients who undergo spinal instrumentation surgery. It is related to altered biome chanics and bone fragility [
2].
To avoid screw loosening or implant failure, several options have been proposed, including adding cement augmentation and variously designed screws such as, expandable screws, bicortical screws, and cannulated and fenestrated screws [
8]. However, when screw loosening or implant failure occurs, few treatment options exist. The typical treatment involves extensive surgery to remove the screws with extension of instrumentation and reinsertion of more pedicle screws adding cage replacement with the addition of allograft or other bone substitutes [
9]. However, all these techniques carry perioperative risks and morbidities and moreover, revision surgery has an expensive cost burden.
Extensive open revision surgery is usually particularly contraindicated for elderly and fragile patients with medical comorbidities. Minimally invasive alternative treatment options using cement augmentation have recently been reported [
5,
6]. They applied a vertebral augmentation technique for pedicle screw loosening to activate screw oversizing and reduce screw micromobility. Cianfoni et al. [
10] also reported percutaneous cement augmentation for the treatment of clinically relevant screw loosening, both in avoidance of extensive open surgery and for pain relief without neurologic complications or clinically significant cement leaks.
However, bone resorption around implants can be caused by infections. In cases of clinical and radiologic suspicion of spinal infection, cement augmentation may be contraindicated. The suboptimal sensitivity of spine biopsies and cultures for low-grade infections remains a challenge in such cases [
11]. Moreover, bone cement augmentation has exothermic properties and leads to frequent complications, such as cement leakage, although most cases are of minor leakages without consequent neurologic deficits.
Xie et al. [
12] reported that augmentation of the pedicle screw with both PMMA and autogenous iliac bone transplant in the treatment of degenerative lumbar scoliosis combined with osteoporosis can achieve good surgical results. No significant differences were found between the autogenous bone chip group and the PMMA group with regard to all aforementioned targets, except for the duration of intake of oral pain medication and cost of surgery. Two patients showed asymptomatic cement leakage during surgery in the cement augmentation group. However, harvesting of the autogenous iliac bone graft can be associated with significant morbidity. Minor complications include persistent pain, superficial seromas, and hematomas. Major complications include herniation of abdominal contents, vascular injury, neurologic injuries, and deep infections at the donor site. Moreover, considering that most patients with screw loosening are in the elderly age-group, autogenous bone harvesting can be particularly traumatic. Considering these points, bone allografts may be an alternative to autogenous iliac bone as the trajectory reinforcement material.
Some researchers have suggested using bone grafts in the screw trajectory to increase the strength of the pedicle screw. However, evidence is limited for improvement in the strength of the pedicle screw with use of bone grafts in the screw trajectory. Pfeifer et al. [
13] used a milled femoral head allograft bone and a matchstick-shaped bone for trajectory revision and found that using bone grafts in the screw trajectory does not improve the strength of the screw in the failed trajectory. Chrea et al. [
14] also utilized allograft bone plugs for trajectory augmentation and found that pullout loads of an augmented screw were not significantly higher than those of an unaugmented screw.
However, recently, Jia et al. [
15] reported that augmentation of the trajectory allograft bone using small-diameter cancellous bone particles via a delivery tube before screw insertion can significantly increase the pullout strength and allowed good distribution of the bone at the screw-bone interface. To improve the bone grafting technique, we used a small allograft of cancellous bone particles and changed the screw trajectory using larger-diameter screws.
In the literature, pedicle screw loosening has been associated with decreased pullout strength and extraction torque. It can be regarded as a type of instrument failure and is related to back pain and pseudoarthrosis [
16].
Therefore, to prevent repeated pedicle screw loosening, we recommend meticulous screw insertion via a new trajectory, using a longer and thicker screw as well as augmentation of allograft bone particles to prevent the toggling effect. In addition, strict care of the spine with osteoporosis or osteopenia is essential.
In our study, we performed removal of the loosened screws, checked the screw channel, and reimplanted larger screws via a new trajectory filled with allograft bone chips. Our technique has the advantage of being a minimally invasive procedure rather than an extensive open surgery, which is conventionally used for treating symptomatic screw loosening. It can also be applied in patients with low-grade local infection, which is a contraindication for cement injection. In the postoperative control at a minimum of 6 months after surgery and at the final follow-up, none of the screws showed significant loosening, and significant pain reduction was maintained.
However, there are some limitations to the current study. The main limitations are the retrospective study design, small sample size short term follow-up, and an intrinsically subjective definition of instrumentation failure. Furthermore, the subjective nature of self-assessment of pain may be another limitation of this study.
Second, we focused on the screw loosening and did not evaluate the interbody fusion status with the status of implanted cages and disc space. A CT scan was not performed after surgery, we are not able to confirm the correct fusion status. It is necessary to perform a CT scan be at least two years after surgery to confirm the fusion status. Therefore, larger, prospective cohort analyses with long-term follow-ups focused on bone fusion status, and biomechanical studies are required to provide more generalized outcome data and to evaluate the long-term results in terms of bone fusion. Moreover, for patients with pronounced, multilevel screw loosening, extensive open revision surgery should be considered. It is of course important to control osteoporosis during the follow-up period.
The current study suggests that reimplantation of pedicle screws via a different trajectory using a larger-diameter screw for selected low-grade screw loosening can provide a well-tolerated alternative to extensive open surgery for select patients.










 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



